What is a herniated disk?
When you experience back pain that shoots down your leg or neck pain that shoots down your arm, everyday activities can become difficult or even intolerable. One cause of neck or back pain is a herniated disk, sometimes called a ‘slipped disk’ or a ‘ruptured disk’.
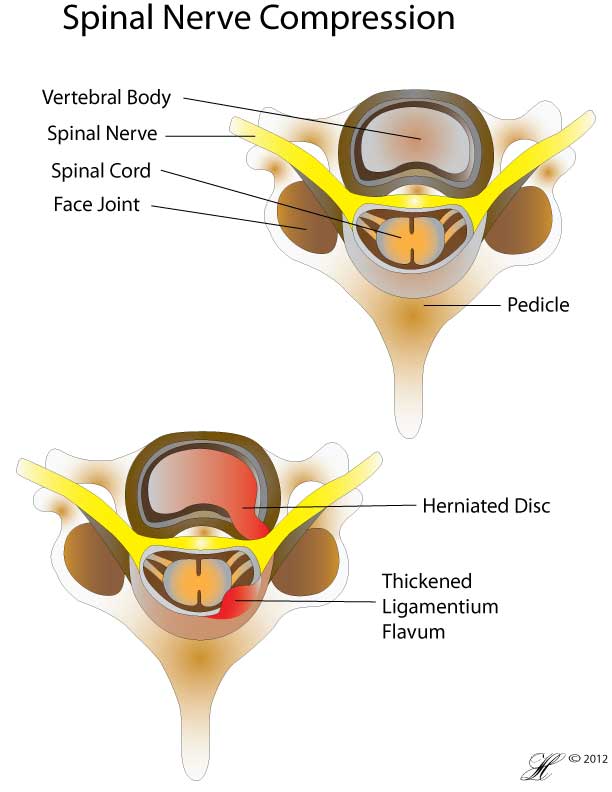
Your spine is made up of block of bones (vertebrae) cushioned by alternating small rubbery oval pads of cartilage or disks. These disks consist of a tough outer layer (annulus) and a soft inner layer (nucleus), like a jelly donut.
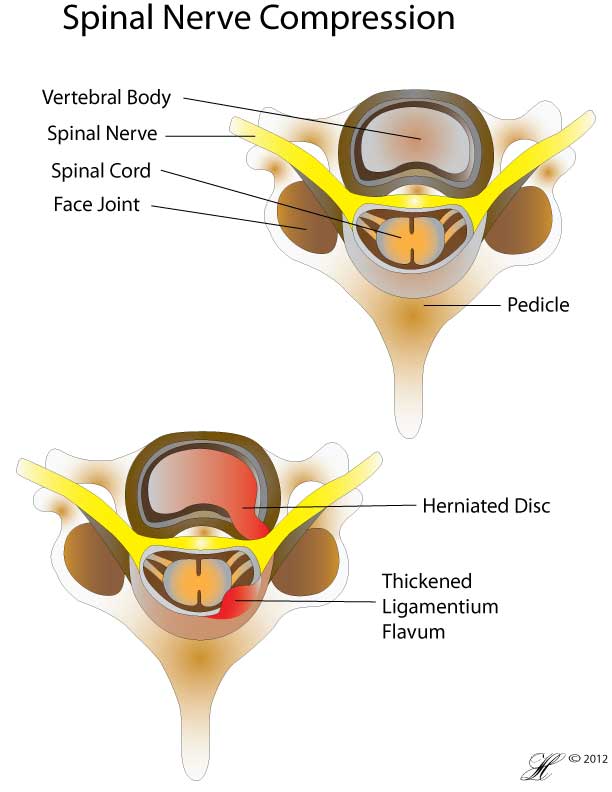
When a herniated disk occurs, a small portion of the nucleus pushes out through a tear in the annulus into the spinal canal. This can irritate a nerve and result in pain, numbness or weakness in your back as well as your leg or arm.
A herniated disk generally gets better with conservative treatment. Surgery for a herniated disk usually isn’t necessary.
Symptoms
Not everyone with a herniated disk experience symptoms from it. They can sometimes be incidental findings on spinal images. However, some herniated disks can be painful.
The most common signs and symptoms of a herniated disk are:
- Sciatica — a radiating, aching pain, sometimes with tingling and numbness, that starts in your buttock and extends down the back or side of one leg.
- Pain, numbness or weakness in your lower back and one leg, or in your neck, shoulder, chest or arm.
- Low back pain or leg pain that worsens when you sit, cough or sneeze.
When to see your doctor
If the pain you experience lasts for more than a week, you should call your doctor to get it checked out.
Back pain often becomes significant enough to interfere with your normal activities for about 1-3 weeks. After that, the pain and disability should improve within 4-6 weeks.
If you’re able to engage in limited activity but see no improvement in three weeks, then call your doctor for an appointment. If the pain increases when you’re sitting, coughing or sneezing, a herniated disk might be the cause.
Visit your nearest emergency department immediately if:
- You lose control of your bladder or bowels.
- Your pain increases rather than staying about the same or decreasing over time.
- You develop numbness or weakness in one or both legs.
When as disc herniation compression several nerves in your spine, it can causes a rare but potentially disabling condition known as cauda equina syndrome. It may require emergency surgery.
Causes
Your spinal column is made up of bones (vertebrae) cushioned by small oval pads of cartilage or disks consisting of a tough outer layer (annulus) and a soft, jelly-like inner layer (nucleus).
These disks act as springs, absorbing shock and allowing bending movements of your spine. They assist your spinal muscles in protecting your spine from the stress of everyday tasks and heavy lifting.
When a herniated disk occurs, a small portion of the nucleus is pushed out through a tear in the annulus into the spinal canal. This situation can cause irritation of one of the spinal nerves.
Disk herniation is most often the result of a gradual, age related wear and tear called degeneration of the disks. As you age, your spinal disks lose some of their water content which make them less flexible and more prone to tearing or rupturing with even a minor strain or twist.
Most people can’t pinpoint the exact cause of their herniated disk. Sometimes, using your back muscles instead of your leg and thigh muscles to lift large, heavy objects can lead to a herniated disk, as can twisting and turning while lifting. Rarely, a traumatic event such as a fall or a blow to the back can cause a herniated disk.
Risk Factors
Several factors make you more susceptible to a herniated disk:
- Age. Herniated disks are most common in middle age, especially between 35 and 45.
- Smoking. Smoking tobacco increases your risk of disk herniation because it decreases oxygen levels in your blood, depriving your body tissues of vital nutrients.
- Weight. Excess body weight causes extra stress on the disks in your lower back.
- Occupations that strain your spine. People with physically demanding jobs have a greater risk of back problems. Repetitive lifting, pulling, pushing, bending sideways and twisting also may increase your risk of a herniated disk. Jobs that require prolonged sitting or standing in one position also may increase your risk of disk herniation.
Investigations
To determine whether you have a herniated disk, your doctor will:
- Ask you questions about your medical history and,
- Perform a physical examination.
Additional possible tests
In most cases, the physical exam is all that’s needed to make a diagnosis. If your doctor suspects another condition or needs to see which nerves are affected, or if there is no improvement after four weeks of conservative treatment, one or more of these diagnostic tests may be performed:
- MRI scan. A magnetic field is used to create images of your body. This test can be used to confirm the location of the herniated disk and to see which nerves are affected.
- CT scan. An X-ray unit creates cross-sectional images of your spinal column and the structures around it.
- X-rays. X-rays don’t detect herniated disks, but they may be performed to rule out other causes of back pain, such as an infection, tumour or a broken bone.
Complications
While it can be painful, a herniated disk isn’t typically a medical emergency. Rarely, disk herniation can cause cauda equina syndrome, which is the compression of spinal nerve roots. Relieving the pressure that causes cauda equina syndrome often requires emergency surgery, because it can cause permanent weakness or paralysis. The following signs and symptoms, which suggest cauda equina syndrome, warrant a trip to the emergency room:
- Significant or increasing pain, numbness or weakness spreading to one or both legs.
- Loss of bladder or/and bowel control or difficulty urinating even with a full bladder.
- Progressive loss of sensation in the inner thighs, back of legs and area around the anus.
Treatment
Rest
The doctor will suggest rest or restricted activity initially but full bed rest for more than a few days is not recommended. The best way to a better recovery is adequate pain control with medications so you can continue to stay active with normal daily activities and do special back exercises. Actions such as lifting, bending, and straining should be avoided.
Exercise
A referral to the physiotherapist will be made by your doctor. He or she will teach you some special exercises you can do to strengthen the muscles in the back to better support your spine and minimise the pain.
Pain medications
A variety of medications can be used to manage your pain. Your doctor will start with the lowest strength medication and work upwards as needed. Some can be bought over the counter at the pharmacy but some will require a prescription.
Steroid injection
For some people, an injection of cortisone (steroid) into the spine will reduce the inflammation around the disk in the back and reduce the pain. This tend to work for up to 3 months. However, not everyone response to the injections.
Surgery
Surgery will be the last resort if all measures above are not successful, except in situations where permanent nerve damage is occuring. Several surgical options exist. Your doctor will refer you to a spine surgical specialist (an orthopedic or neurosurgeon) to discuss which option is best for you and what the likelihood of success will be.
Seeking Advice
Your Family Doctor (GP)
Your Family Doctor will be able to diagnose and help treat your problem. He or she will be able to
- tell you about your problem
- advise you of the best treatment methods
- prescribe you medications
- and if necessary, refer you to Specialists (Consultants) for further treatment
Prevention
To help prevent a herniated disk:
- Exercise. Regular exercise slows age related degeneration of the disks, and core-muscle strengthening helps stabilise and support the spine. Check with your doctor before resuming high-impact activities such as jogging, tennis and high-impact aerobics.
- Maintain good posture. Good posture reduces the pressure on your spine and disks. Keep your back straight and aligned, particularly when sitting for longer periods. Also, lift heavy objects properly, making your legs — not your back — do most of the work.
- Maintain a healthy weight. Excess weight puts more pressure on the spine and disks, making them more susceptible to herniation.
- Quit smoking. Smoking increase your risk of back problems.
F.A.Q. | Frequently Asked Questions
What can I do to treat a herniated disc at home?
- Relax. Find a comfortable position for rest. Some people are comfortable on the floor or a medium-firm bed with a small pillow under their head and another under their knees. Some people prefer to lie on their side with a pillow between their knees. Don’t stay in one position for too long.
- Walk. Take a short walk (10 to 20 minutes) on a level surface (no slopes, hills, or stairs) every 2 to 3 hours. Walk only distances you can manage without pain, especially leg pain.
- Take pain medicine if needed. These medicines usually work best if you take them on a regular schedule instead of waiting until the pain is severe.
- Try heat or ice. Try using a heating pad on a low or medium setting for 15 to 20 minutes every 2 to 3 hours. Try a warm shower in place of one session with the heating pad. Or you can buy single-use heat wraps that last up to 8 hours. You can also try an ice pack for 10 to 15 minutes every 2 to 3 hours. You can use an ice pack or a bag of frozen vegetables wrapped in a thin towel. There is not strong evidence that either heat or ice will help, but you can try them to see if they help. You may also want to try switching between heat and cold.
