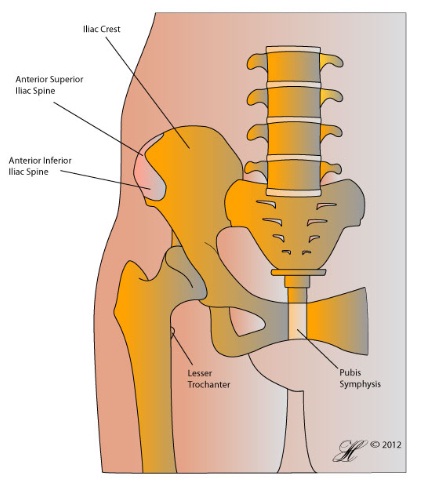
Ankylosing spondylitis is an inflammatory disease that cause pain primarily in the joints of the spine and pelvis (buttock area).
The exact cause of ankylosing spondylitis is currently unknown but a strong hereditary component has been observed. Unlike other causes of back and joint pains, it is not associated with wear and tear or particular jobs or lifestyle choices.
Ankylosing spondylitis tends to progress overtime to other joints and other parts of the body but early intervention can dramatically reduce the impact it has on quality of life.
Symptoms
People with ankylosing spondylitis experience different symptoms and of varying severity.
The main symptoms are stiffness and an aching-type pain in the lower back and buttocks. The pain usually develops overtime or comes and goes in episodes. Both the stiffness and back pain will usually improve with exercise but tend to be worse in the morning. The pain may wake you up at night.
Additional symptoms that you may or may not experience include:
- Lethargy, general unwellness, recurrent bouts of mild fever.
- Pain and swelling in other joints eg. hip, shoulder, kneecap, below the heel.
- Red and sore eyes and problems with vision due to inflammation in the eye (iritis). Damage will become permanent if left untreated.
- Diarrhoea and bloating caused by inflammation of the stomach lining (inflammatory bowel disease).
- Focal pain on the chest due to inflammation of the rib-ligament joints (enthesitis).
- White-scaly rashes (psoriasis) on the skin around your elbow and/or knees.
Causes
Although the cause of ankylosing spondylitis is not yet understood, but we do know that genetics play a key role in the development of this disease. A gene that produces the protein HLA-B27 has been found in many people who have ankylosing spondylitis, however it is important to note you don’t need to have this gene to develop the disease and not everyone with the gene will show any symptoms.
It is thought to be a combination of genetic predisposition and an environmental trigger.
Risk Factors
Ankylosing Spondylitis can affect anyone at any age, but tends to affect:
- Young men aged 15 to 40
- People with a family history of ankylosing spondylitis or other forms of inflammatory arthritis like psoriatic arthritis.
Investigations
Ankylosing spondylitis is diagnosed with a combination of blood tests and X-Rays.
In addition to getting X-Rays of your lower back, your doctor may request X-Rays of your upper spine and neck. If you have symptoms affecting other joints in your body, like your hips or shoulders, you may also need X-Rays of these joints.
If your doctor is concerned about your ankylosing spondylitis affecting other organs in your body, you may need tests for these areas including:
- Chest X-Ray
- Blood tests
Complications
There are a number of complications that may follow ankylosing spondylitis. These may be related to:
- The effect of the disease has on organs in your body, in particular your heart, lungs and kidneys.
- The effect of medications:
- Steroids (prednisolone). Although not always used to treat ankylosing spondylitis, they may be used from time to time. Common SEs include thinning of the bones, gaining weight and mood disturbance.
- Specialist medications – these have a number of side effects, including nausea, vomiting and drowsiness. More seriously, they can increase the risk of serious infection, and mildly increase the risk of developing some rare cancers.
- The effects of fusion of the spine. Most importantly, there is an increased risk of vertebral fractures and reduced lung capacity from kyphosis (excessive curving of the spine).
- Rare but serious complications of the deformity in the spine include effects on the spinal cord, including the development of cauda equina syndrome. In the neck or cervical spine, instability of the upper vertebra (C1 & C2) is a potentially dangerous complications.
- The effects of ankylosing spondylitis on other joints in the body:
- The hip and shoulder may become increasingly painful, eventually requiring surgery.
- The large tendons affected by ankylosing spondylitis, like the Achilles tendon, are more prone to rupture (see Achilles Tendon Rupture).
Treatment
The treatment of ankylosing spondylitis varies depending on how aggressive the disease and when the diagnosis is made.
Mild Ankylosing Spondylitis in the Early Phase
The initial treatment for ankylosing spondylitis is aimed at relieving the symptoms of pain and slowing the progress of the inflammation. Over the counter anti-inflammatory medications like ibuprofen are very effective at controlling pain and reducing inflammation.
As time goes past, braces and physical therapy that maintain the normal posture of the spine can prevent the fusion of the spine in a deformed position. This greatly assists with breathing and movement.
- At all stages of ankylosing spondylitis, physical therapy and exercise can be very beneficial in reducing symptoms and maintaining the flexibility in the spine.
Physiotherapy will focus on:
- Maintaining your posture.
- Breathing exercises that keep your lungs inflated.
As your ankylosing spondylitis develops you may need to see a rheumatologist, who can prescribe:
- Stronger anti-inflammatory medications, like steroids. These are not usually used for the spinal symptoms of ankylosing spondylitis but can be helpful in controlling the symptoms in the hip, shoulder and other joints.
- Specialist medications. There are a number of different medications that can be used to treat the symptoms and slow the progression of ankylosing spondylitis, usually from the class of drugs known as ‘TNF-alpha inhibitors’. These medications reduce the ability of your immune system to attack the ligaments and joints.
Ankylosing Spondylitis with Deformity
When AS has been present for some time and the spine has already begun to fuse, braces and physical therapy will do little if anything to reverse the deformity of the spine.
Surgery may be considered when the deformity is:
- Significantly affecting quality of life, for example impacting the ability to work or perform simple tasks like eating.
- Putting you at serious risk, for example, the development of tingling and numbness in the lower limbs may suggest the deformity is now impinging on the spinal cord.
Alternatively, surgery may be necessary when there is a fracture in the spine.
In all the above situations, the aim of surgery is to stabilise the spine in a functional position – not to make it flexible again. The standard surgical option for ankylosing spondylitis is osteotomy or reshaping and trimming of bones. This is usually combined with fusion (see Lumbar Spinal Fusion and Cervical Spinal Fusion).
After these operations, you may need to keep your back / neck still for some time as the bones heal over the screws.
Ankylosing Spondylitis and Other Joints
Other joints may be seriously affected by ankylosing spondylitis. The symptoms in joints like the hip and shoulder, feet and knees should also be controlled by medications. When these joints are seriously affected, surgery may be considered. Surgical options may include:
- Hip replacement or hip fusion.
- Shoulder replacement or fusion.
- Arthroscopy and debridement of joints in the feet.
Seeking Advice
Your Family Doctor (GP)
Your Family Doctor will be able to diagnose and help treat your problem. He or she will be able to
- tell you about your problem
- advise you of the best treatment methods
- prescribe you medications
- and if necessary, refer you to Specialists (Consultants) for further treatment.
Usually, ankylosing spondylitis is treated by specialist doctors called rheumatologists. These doctors can:
- confirm the diagnosis of AS
- prescribe stronger medications and injections when needed
- give you advice on how to prevent complications from your disease
For more information on rheumatology and rheumatoid conditions:
- The Australian Rheumatology Association provides patient-centred information on ankylosing spondylitis, as well as a number of other conditions and the medications commonly used to treat them.*
*Orthoanswer is not responsible for information provided at external sites.
Prevention
If you are aware of family members with inflammatory arthritis, you can try to be aware of changes of flexibility in your lower spine and seek medical attention early.
This is usually not a realistic method of prevention. If you are very concerned about developing this disease there are genetic tests that confirm if you have a gene strongly related to ankylosing spondylitis.
If you have a diagnosis of ankylosing spondylitis and wish to prevent complications, you should:
- Stay active, exercising regularly and when appropriate using physical therapy to maintain your posture.
- Stop smoking – the importance of preserving lung function cannot be overemphasised in ankylosing spondylitis. Talk to your GP about Quit programs and medications if you are struggling to stop smoking.
- Take medications and anti-inflammatories as prescribed by your doctor.
- Wear spine braces early in the disease. These can be worn at night.
F.A.Q. | Frequently Asked Questions
Does pregnancy in an individual with Ankylosing Spondylitis cause any complication to the mother or her baby?
It does not involve any problem for mother or baby , however some medications taken by the mother can be harmful to the baby. Consult and discuss with your doctor.
Is Anemia, an indication for Ankylosing Spondylitis?
No, anaemia is a disease where there is a deficiency of haemoglobin in the blood. It can be treated either by medication or blood transfusion (if necessary).In Ankylosing Spondylitis, anaemia is an associated symptom, as the general constitution of the body is affected.
References
Braun, J. and J. Sieper (2007). “Ankylosing spondylitis.” The Lancet 369(9570): 1379-1390.
Hellman, D. B., Imboden, J. B., ‘Chapter 20. Musculoskeletal & Immunologic Disorders’ in McPhee, S. J. et al. (Eds), CURRENT Medical Diagnosis & Treatment 2012, Retrieved from Access Medicine on 29-Sept-2011.
Humphreys, S. C., ‘Ankylosing Spondylitis in Orthopedic Surgery’, Medscape Reference, Accessed 29-Sept-2011 from http://emedicine.medscape.com/article/1263287-overview.
Gorman J.D., Imboden J.B., ‘Chapter 17. Ankylosing Spondylitis and the Arthritis of Inflammatory Bowel Disease’, in J.B. Imboden, et al. (Eds), CURRENT Rheumatology Diagnosis & Treatment, 2e, 2011, retrieved from Access Medicine on 29-Sept-2011.
