A Total Knee Replacement is a very common operation to help relieve pain and stiffness in the knee joint. It is a very effective operation for people with long term knee pain due to conditions such as osteoarthritis.
During a knee replacement operation, the diseased knee joint is removed and replaced with an artificial joint.
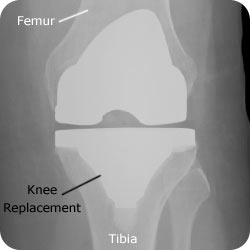
Diagram of a knee with a Total Knee Replacement (uncemented variety)
Who is this operation for?
A Total Knee Replacement is for patients who have severe pain and stiffness in the knee.
You may benefit from knee replacement surgery, if:
- Your knee pain is severe.
- The pain is present at night and at rest.
- It limits your movements and activities such as walking and climbing stairs.
- It affects your ability to look after yourself such as showering or putting on shoes.
- You have tried non-surgical alternatives without success.
The most common cause of knee pain leading to a knee replacement is osteoarthritis. This is also known as ‘wear and tear’. Other causes include:
- Rheumatoid arthritis
- Knee trauma (accidents leading to breaks in the bone near the knee joint).
- Infection
(follow the links for more information on these conditions)
Diagram of a knee with Osteoarthritis
Alternatives to surgery
Surgery may be necessary if your symptoms are severe. There are however some alternatives to surgery which may help with the symptoms caused by the knee problem. These include:
Pain-relief medications – such as paracetamol
Anti-inflammatory medications – these medications can be harmful if used long term and you should discuss the use of these medications with your doctor before starting
Walking aids – such as walking sticks or frames
Physiotherapy – exercises to improve muscle strength may help with mobility and reduce pain
Weight loss – being over weight can make your knee pain worse. Loosing weight can help reduce pain and also lead to better results if you have the operation.
Benefits of the operation
A knee joint replacement is usually a very successful operation and will help to:
- Reduce pain
- Improve mobility: You should be able to move about more freely after your knee operation.
- Improve your quality of life: With less pain and better mobility, you be able to carry out your daily tasks more easily.

A Xray of the Left Knee showing Osteoarthritis

A Xray of the Right Knee showing normal anatomy
What can you expect to be able to do after a knee joint replacement?
It is important to understand what a knee replacement can and cannot do before deciding to have the operation.
After the knee replacement operation, most patients are able to return to gentle exercise such as:
- Walking
- Swimming
- Golfing
- Dancing
- Bike riding (gentle riding)
High impact sports are not recommended after a knee replacement. These activities can place too much stress on the knee and lead to early wear and tear of the knee replacement. High impact sports which are not recommended include:
- Running
- Football
- Basketball
- Martial arts
- Squash
- Water skiing / down hill skiing
Complications
Side effects:
Side effects are symptoms that occur after every operation and are a normal part of the recovery from the operation. The main side effects which may last for several weeks after knee replacement surgery are:
- A sore knee
- Swelling and bruising around the knee
- Stiffness of the knee
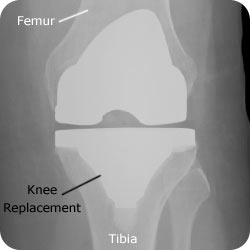
Xray of a knee with a total knee replacement (cemented variety)
Complications
Complications are uncommon problems that occur during or after the operation. Most people having knee surgery aren’t affected.
The general complications for all operations are:
- A reaction to the anaesthetic
- Infection of the wound or joint
- Excessive blood loss
- A blood clot, usually in a vein of the leg (known as a deep vein thrombosis or DVT)
Complications that are specific for total knee replacement surgery include:
- Ongoing knee pain: The main reason for having a knee replacement is persistent knee pain. A knee replacement is usually a very effective method of relieving knee pain. It is important to know however that a small number of patients have ongoing knee pain after their operation. Between 6- 17% of patients having a knee replacement will have ongoing pain after their operation.
- Nerve damage: Nerves can be injured during the operation. The chance of getting nerve injury is very low.
- Stiffness. Stiffness of the knee after surgery can occur and it is important to work hard on your rehab exercises to minimise this problem.
- Wearing out of the replaced knee: Although you have a new knee after your procedure it still undergoes wear and tear due to your everyday activities. 94% – 97% of knee replacements will last at least 12 years
- Dislocation: Very rarely after your operation your knee can become unstable and actually dislocate or pop out of place.
- Fracture: During or after your knee replacement there is a small chance that the bones around the metal can break.
The Operation
The operation usually takes around 2 hours.
Your surgeon will make an incision that is typically around 15 – 25 cm. It usually runs straight down the middle of the front of your knee.
Precise surgical bone cuts are made at the end of your femur (thigh bone) and the top of your tibia (shin bone), thereby removing your arthritic knee joint.
The knee replacement is made of surgical-grade metal alloy and plastic.
It is inserted and held in place either by surgical cement, a special coating on the metal or screws.
Before the operation
Preadmission Clinic | Preparing for Surgery
Before your operation, you will be seen at the Preadmission clinic to make sure you are fit for the operation and all the necessary tests are performed in preparation for the operation.
During the visit, you will be seen by a
- doctor
- nurse
- anaesthetist (if necessary)
You may also need to have a specialised anaesthetic assessment.
Tests
Tests that may be ordered for you include:
- blood tests
- Xray knee
- Xray of your Chest
- Urine Test
- ECG
Preparing Your Skin
Your skin should not have any infections or irritations before surgery. If either is present, contact your orthopaedic surgeon for a program to improve your skin before surgery.
Tip
Carry a list of your medications with you including the name, dosage and how often you take it.
Medications
Our doctors will advise you which medications you should stop or can continue taking before surgery.
 Go see your dentist
Go see your dentist
Consider getting treatment for significant dental diseases (including tooth extractions and periodontal work) before your knee replacement surgery. Routine cleaning of your teeth should be delayed for several weeks after surgery.
Get some help from your friends and family
Although you will be able to walk with crutches or a walker soon after surgery, you will need some help for several weeks with such tasks as cooking, shopping, bathing, and laundry. If you live alone, your orthopaedic surgeon’s office, a social worker, or a discharge planner at the hospital can help you make advance arrangements to have someone assist you at your home. A short stay in an extended-care facility during your recovery after surgery also may be arranged.
Home Planning
The following is a list of home modifications that will make your return home easier during your recovery:
- Securely fastened safety bars or handrails in your shower or bath
- Secure handrails along all stairways
- A stable chair for your early recovery with a firm seat cushion, a firm back, and two arms
- A raised toilet seat
- A stable shower bench or chair for bathing
- A long-handled sponge and shower hose
- Try and get some shoes which have no laces
- Place items you use regularly at home at arm level so you do not have to reach up or bend down.
- A grabbing tool that will allow you to grab objects without excessive bending of your knees
- Removal of all loose carpets and electrical cords from the areas where you walk in your home
Admission
Most people are admitted to hospital on the day of their surgery.
Anaesthesia
The anaesthetic team will see you and decide the type of anaesthetic that’s best for you.
The different types of anaesthesia include:
- General Anaesthetic. This type of anaesthetic puts you asleep during the whole procedure and a machine controls your breathing.
- Spinal Anaesthetic. An injection is placed into your back to numb your legs. You will be awake during the procedure, however a sedative can be given to you to help you doze off.
- Nerve Blocks. This special injection is used to help with your pain after the operation and often used in conjunction with a general anaesthetic.
Recovery Room
After the operation, you will be resting in the recovery room, where specially trained nurses will closely monitor you. This usually takes 1 to 2 hours. After which, you will be taken to your hospital room.
After the Operation
Immediately after the operation
You will wake up in the recovery area after the operation is completed. You may not be able to feel or move your leg for the next few hours due to the anaesthetic you have just had. You may need to have some painkillers after the anaesthetic wears off, as the knee will be sore following the operation.
Day 1
You will have a blood test to check your blood levels and an X-ray to check the knee replacement is sitting correctly.
The wound will be checked and you will be given painkillers to manage the pain after the operation.
The physiotherapist will come to see you and give you simple exercises to start your recovery from the operation as early as the same day. They will help you to sit up and bending your knee and walking immediately with walking aids such as crutches or a frame.
During your hospital stay
Whilst in hospital you will be monitored to ensure there are no complications from your operation and that you are medically stable. Most people walk with assistance on day 1 after their operation.
You will continue to see the physiotherapist daily who will prescribe exercises and help you to get back on your feet and walking. Often after the operation, you may need a frame to walk with in the early phases of recovery and you will probably go home with crutches.
Whilst in hospital you will also be seen by the occupational therapist. They will help you to make sure that you will be safe at home by doing all the simple things that are often more difficult after an operation like showering, getting out of bed and moving around in the house.
The physiotherapist, occupational therapist and your doctors will discuss with you whether you can go straight home after your hospital stay or whether you need to have some time with the rehabilitation team in the hospital. The rehabilitation team will help people who are slow to recover. They will build up your strength and improve your walking before returning to home.
Most people who are fit and well before their operation only stay in hospital for 1-2 days after their operation. If you have several other medical problems or you are slow to recover, your hospital stay may be longer. You will need to stay in the hospital until you are able to walk safely, often with crutches and your pain is well controlled.
Recovery and Rehabilitation
How long will it take to recover?
It takes about 3 months to recover from this operation. You will be given exercises to do for a month after your surgery. You will also be shown how to safely climb stairs, shower, dress and toilet yourself.
It is important to follow the advice of your surgeon and physiotherapist in order to ensure the recovery goes smoothly.
Wound Care | How do I look after my wound?
It is important to keep your wound as dry as possible.
Most patients are discharged home with a waterproof dressing, which can be left on for showering.
During the first 24 hours, it is normal to have some minor bleeding. After being discharged home, there should be no discharge, redness or bleeding around the wound.

If there is redness, discharge or a foul odour, please seek medical attention as soon as possible.
Wound Care | When will my stitches be removed?
There are several ways your wounds may be closed.
You may have either have
- non-absorbable stitches
- absorbable stitches
- surgical staples.
The stitches or staples are usually removed 10-14 days after surgery.
Diet | What should I eat and drink?
There is usually no specific diet or extra vitamins/nutrients needed to recover from a total knee replacement operation.
It is important to have a normal healthy balanced diet and plenty of nonalcoholic fluids.
Activity | What exercises should I do at home?
Physiotherapy and the exercises that you perform at home are extremely important to achieve the best results after a knee replacement.
After returning home, you should gradually be able to do more and more. It is important to look after your new knee and follow your surgeon’s and physiotherapy instructions.
Your program may include exercises that work on your:
- walking
- sitting
- stair climbing
- muscle strength
Avoiding Falls
A fall during the first few weeks after surgery can damage your new knee and may result in a need for more surgery.
Be careful on Stairs. Stairs are a particular hazard until your knee is strong and mobile, and you’ve regained your balance. You should use a walking aid such as a cane, crutches, or a walker. Use the handrails on your stairs or ask for someone to help you., or handrails or have someone help you.
Looking after my knee joint
Joint replacements can become infected at any time after the surgery from the first postoperative day to many years down the line.
You can take the following steps to help prevent infection:
- Take antibiotics before dental or any medical procedure.
- See your doctor to treat all suspected urinary tract infections.
- Look for signs of infection in the knee including pain, redness, swelling or increased warmth.
- Your new joint replacement may trigger airport metal detector alarms. We will give you a certificate that verifies that you had a knee replacement.
- Keep in mind that you need to protect your knee replacement to ensure a long-lasting, successful result. Follow all instructions concerning any activity restrictions.
F.A.Q.s | Frequently Asked Questions
What are the alternative treatments to having a knee replacement?
Walking aids such as a walking stick. An exercise program can strengthen the muscles around the knee joint and sometimes improve the positioning of the knee and relieve pain.
- Nonsteroidal anti-inflammatory drugs, or NSAIDs. Some common NSAIDs are aspirin, ibuprofen and Celebrex.
- Corticosteroids such as prednisone or cortisone reduce joint inflammation but can cause further weaken the bones in the joint. Side effects from corticosteroids are increased appetite, weight gain, and lower resistance to infections.
- Osteotomy. The surgeon cuts the bone away at a point from the damaged joint and restores the joint to its proper position, which helps to load weight evenly across the joint. For some people, an osteotomy relieves pain. Recovery from an osteotomy takes 6 to 12 months. The function of the knee joint may get worse and the patient may need more treatment.
Are there important things I need to tell my doctors?
- Redness, swelling or warmth around the cut
- Leakage from the cut
- Fever and chills.
- Severe knee pain that is not relieved by prescribed painkillers.
- Sudden sharp pain and clicking or popping sound in the knee joint
- Loss of control over leg movement
- Loss of leg movement
- Further surgery planned for the future i.e. dental work, bladder catheterisation, examinations of the bowel, bladder, rectum or stomach.
What are the bones of the knee?
The knee is a hinge joint, formed by the end of the thighbone (femur) and the end of the shin bone (tibia). The bones are coated in cartilage, which acts as a cushion between the two bones and allows the knee to move. In front of these bones is the kneecap (patella) which glides in a groove on the end of the thigh bone.
Diagram of the bones and ligaments of the knee
