The Posterior Cruciate Ligament (PCL) is a ligament located around the back of your knee. It connects you thigh bone (femur) to your shin bone (tibia). It stabilises your knee and allows it to function properly. It is actually one of the strongest ligaments in your knee.
The PCL injury mainly refers to your PCL being torn or stretched.
The PCL is torn much less commonly than the Anterior Cruciate Ligament (ACL) and usually causes much less problems.
If the PCL is torn without any other structures being injured in the knee, it can often be treated by exercises and physiotherapy.
Symptoms
Signs and symptoms of a posterior cruciate ligament injury may include:
- Pain in your knee especially when using it ie walking, running, jumping
- Rapid knee swelling and tenderness (within three hours of the injury)
- Instability of your knee
- Knee gives way
- Pain with kneeling or squatting
- A slight limp or difficulty walking
Most people with a posterior cruciate ligament injury don’t feel a “pop” at the time of injury which is the classic sign of an ACL tear. Signs and symptoms may be mild or vague, and you might not even notice anything wrong. Over time, the pain may worsen and your knee may feel more unstable. If other parts of the knee are affected, your signs and symptoms will likely be more severe.
Causes
The posterior cruciate ligament is usually injured if your knee becomes overextended or if you knee is struck while it is bent. This happens commonly in motor vehicle accidents, when the a persons’ bent knee is smashed against the dashboard, and so the shinbone is pushed back causing the posterior cruciate ligament to tear. Also PCL injury can occur in contact sports like football or soccer. It happens because they can fall on their bent knee which can cause the PCL to tear or stretch.
Risk Factors
The main risk factors for PCL injury are if you are male and what type of sports you play. Males have a higher chance than women of injuring their PCL, and contact sports increase your likelihood of having a PCL tear.
Investigations
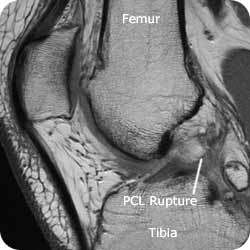
A MRI showing a ruptured PCL
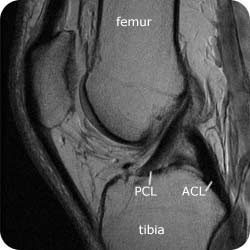
A MRI showing normal knee anatomy and an intact PCL
X-ray: Although an X-ray isn’t very good at picking up ligament damage, it can reveal bone fractures. People with posterior cruciate ligament injuries sometimes have fractures where a small chunk of bone attached to the PCL, pulls away from the main bone.
Magnetic resonance imaging (MRI): This painless procedure uses magnetic fields to create computer images of the soft tissues of your body. An MRI scan can clearly show a posterior cruciate ligament tear and determine if other knee ligaments or cartilage also are injured.
Arthroscopy: If it’s unclear how extensive your knee injury is, your doctor may use a surgical technique called arthroscopy to look inside your knee joint. A small, lighted optic tube is inserted into your knee joint through a small incision. The doctor views images of the inside of the joint on a computer monitor or TV screen.
Complications
In a lot of people, other structures within the knee like other ligaments, cartilage and bone are damaged when you have a posterior cruciate ligament injury. Depending on how many of these structures were damaged, you may experience some long-term knee pain and instability.
You may also be at higher risk of eventually developing arthritis in your affected knee.
Treatment
What treatment is best depends on the extent of your injury and whether it just happened or you’ve had it for a while.
Medications
Nonsteroidal anti-inflammatories, such as ibuprofen or can help relieve pain and reduce swelling.
Therapies
- P.R.I.C.E. Mild to moderate joint injuries often are helped by following the P.R.I.C.E. model — protection, rest, ice, compression and elevation.
- Physiotherapy. A physiotherapist can teach you exercises that will help make your knee stronger and improve its function. You may also need a knee brace or crutches during your rehabilitation.
Surgical or other procedures
- Joint aspiration. This procedure uses a syringe to remove fluid from the joint. Aspiration may be performed if you have significant swelling of the knee that interferes with the joint’s range of motion and your ability to use your knee or leg muscles.
- Surgery. If your injury is severe — especially if it’s combined with other torn knee ligaments, cartilage damage or a broken bone — you may need surgery to reconstruct the joint. Surgery might also be recommended if you have persistent episodes of knee instability despite rehabilitation.
Looking After Yourself
- Rest your injured knee and protect it from further damage. You may need to use crutches.
- Apply ice packs to your knee for 20 to 30 minutes every three to four hours for two to three days or until the pain goes away.
- Elevate your knee by placing a pillow underneath it.
- Take pain relievers such as ibuprofen as needed.
- Wrap an elastic bandage around your knee.
Seeking Advice
Your Family Doctor (GP)
Your Family Doctor will be able to diagnose and help treat your problem. He or she will be able to
- tell you about your problem
- advise you of the best treatment methods
- prescribe you medications
- and if necessary, refer you to Specialists (Consultants) for further treatment
If your knee injury is severe, you may need to seek emergency medical care. In some cases, however, you may initially consult your family doctor (GP). He or she may refer you to a doctor who specializes in knee injuries or sports medicine.
Bring along information about yourself
It can be a great help for your doctor if you bring along the following information about yourself
- A list of your medications, including the name and dosage.
- Information about your medical problems and past treatment
- Previous investigation results, such as xrays and blood tests.
Prepare a list of questions for your doctor
You may want to write a list that includes:
- Detailed descriptions of your symptoms
- Information about medical problems you’ve had in the past
- Information about the medical problems of your parents or siblings
- All the medications and dietary supplements you take
- Questions you want to ask the doctor
What to expect from your doctor
- Medical history. Your doctor will ask about the accident or injury, the problems you’re having with your knee, how long you’ve had symptoms, and whether you have a history of knee injuries.
- Physical examination of the knee. Your doctor may press on your knee to feel for injury, looseness or fluid in the joint from bleeding. He or she may move your knee, leg or foot in different directions and ask you to stand and walk to see if your knee stays in proper position. Your doctor will compare your injured leg with the healthy one to look for any sagging or abnormal movement in the knee or shinbone.
- Posterior drawer test. In this test, you lie on your back with your knee bent. Your doctor gently moves your lower leg backward at the knee. If the leg moves back excessively, your posterior cruciate ligament may be torn.
Prevention
The main way to prevent this type of injury is to use the right technique when playing sports. Also being safe on the roads prevents this sort of injury and many other forms of injury. Nevertheless, PCL injury is often unpreventable.
F.A.Q. | Frequently Asked Questions
When will I feel better after a torn knee ligament?
Recovery time depends on how severe your knee ligament injury is. People also heal at different rates. While you recover — If your doctor agrees — you could take up a new activity that won’t hurt your knee. For instance, runners could try swimming.
Whatever you do, don’t rush things. Don’t try to return to your old level of physical activity until:
- You feel no pain when you bend or straighten your knee.
- You feel no pain in your knee when you walk, jog, sprint, or jump.
- Your knee is no longer swollen.
- Your knee feels as strong as your uninjured knee.
If you start using your knee before it’s healed, you could cause permanent damage.
