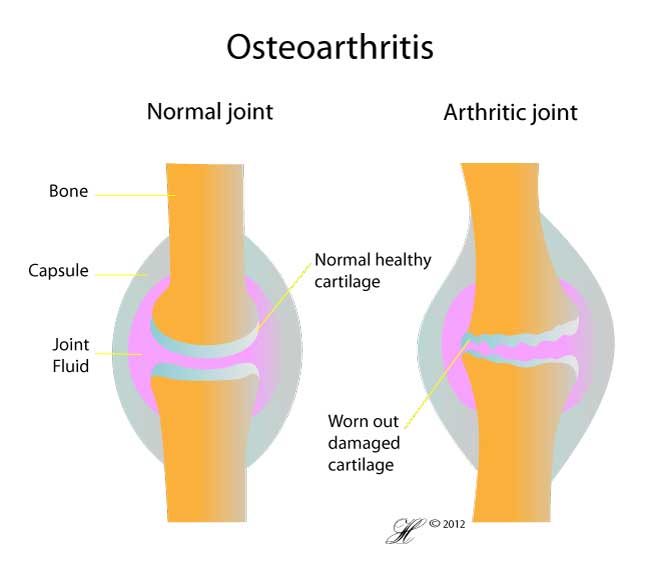
Osteoarthritis is usually a slowly progressive degenerative disease in which the joint cartilage gradually wears away. Your joint cartilage, also called articular cartilage, is a smooth glistening surface that allows your joint to move smoothly with low friction.
Osteoarthritis most often affects middle-aged and older people. However, if can also affect young people if the joint cartilage has been damaged or weakened, such as in an injury.
Symptoms
The main symptom you may have is a deep aching pain in your joint which is worse on movement. Other things you may notice are:
- Your knee looks red and swollen
- Your knee feels stiff, especially in the morning
- A grinding or crunching sound when you move your knee
- You may notice your legs look bowed/curved
- You may get a limp
- You may feel your knee locks or buckles
Symptoms can vary greatly from patient to patient, with some having very mild symptoms to others suffering from severe OA
Causes
OA is a degenerative condition which manifests itself over many years, so you will see it mainly in older people. However, there are some factors which cause it to occur early:
- Acute knee injury. This includes trauma to the knee which causes damage to the cartilage
- Knee conditions. Such as rheumatoid arthritis and gout which damage the cartilage
- Weight and overuse. Both these place stress on the knee causing the cartilage to wear away
Risk Factors
The risk factors of OA of the knee include:
- Age-The older you are the more likely you are of getting it. In the US one third of people over 65 have it
- Gender-Women are more likely to get it than men
- Weight-Those who are obese are putting more stress on their knees, causing increased wear and tear of the joint and thus more likely getting OA
- Injury-Acute knee injury predisposes for OA
- Deformity-Congentical or acquired deformity of the hip or knee can lead to premature OA
- Occupation-Certain jobs place people at increased risk of OA eg. Farmers, Jackhammer operators
- Muscle-Weak thigh muscles can lead to OA of the knee
- Knee disease-Conditions like gout and rheumatoid arthritis can predispose for OA
- Vitamins-Low intakes of vit D and vit C has been linked with higher rates of knee OA
Investigations
Usually your doctor can diagnose your knee arthritis without any investigations. However, an x-ray may be done and this can show a narrowed space between your knee bones which indicates osteoarthritis. Sometimes blood tests, an MRI or a bone scan may be done to determine the state of the surrounding soft tissue if surgery is being considered. If your knee is swollen with fluid, sometimes it may be aspirated so the fluid can be tested on.
Complications
There are a couple of complications that can occur due to OA of the knee. One is deposition of calcium crystals in the cartilage called chondrocalcinosis. OA flares up when there are crystals present, causing increased pain and swelling. Crystals can occur in any joint with or without OA but is much more common to be seen in a knee with OA. Another complication that can occur due to OA is the formation of cysts behind knee. These are known as Bakers cysts. They are soft lumps felt behind the knee which are usually painless but can ache during exercise. These cysts can press on blood vessels causing leg swelling, or the cyst can burst causing pain. Cysts are usually treated by aspiration of the fluid.
Treatment
OA is a condition which generally cannot be cured short of replacing the joint, so the goal of treatment is to reduce pain and maintain mobility.
First measures include weight reduction and pain management with simple pain-killers. Avoid activities which aggravate the knee such as jumping or running and do sports like swimming or cycling. You can go to a physical therapist which increases the strength in your legs. You can also use supporting equipment such as knee braces, a walking stick, shoe inserts or energy absorbing shoes.
Sometimes simple pain-killers aren’t enough and the doctor may offer you alternative treatments such as glucosamine, NSAIDS or steroid injections.
However, if despite all these measures you still experience unbearable pain and have great difficulty coping with your day to day activities, surgery may be recommended.
The surgical options available are:
- Knee arthroscopy which is used to clear debris or repair torn cartilage
- An osteotomy which is where your bones are cut to make the knee joint more straight and properly aligned
- A total knee replacement or partial knee replacement where your knee is replaced by an artificial joint
- Cartilage from elsewhere on your body can be grafted into the deficient part of your knee
Seeking Advice
Your Family Doctor (GP)
Your Family Doctor will be able to diagnose and help treat your problem. He or she will be able to
- tell you about your problem
- advise you of the best treatment methods
- prescribe you medications
- and if necessary, refer you to Specialists (Consultants) for further treatment
Prevention
Things that can be done to reduce you chance of getting OA
- Maintain your ideal body weight
- Exercise regularly
- Protect jour joints by having a good posture
- Avoid repeated stress on your knees
- Listen to your pain, if your knee hurts when you do something, don’t do it
- Avoid direct injury to your knees
F.A.Q. | Frequently Asked Questions
Is osteoarthritis and osteoporosis the same?
No, osteoarthritis is degeneration of the cartilage while osteoporosis is thinning of the bone which leads to the bone being more likely to fracture.
