The right hip has a Total Hip Replacement and the left hip is normal.
A Total Hip Replacement is a very common operation to help relieve pain and stiffness in the hip joint. It is a very effective operation for people with long term hip pain due to conditions such as osteoarthritis, also known as ‘wear and tear’.
During a hip replacement operation, the diseased hip joint is removed and replaced with an artificial joint.
Is hip replacement surgery for you?
A Total Hip Replacement is for patients who have severe pain and stiffness in the hip.
You may benefit from hip replacement surgery if:
- Your hip pain is severe.
- The pain is present at night and at rest.
- It limits your movements and activities such as walking and climbing stairs.
- It affects your ability to look after yourself such as showering and putting on shoes.
- You have tried non-surgical alternatives without success.

The Right Hip has been affected by Osteoarthritis
What are the alternatives to surgery
Surgery may be necessary if your symptoms are severe. There are however some alternatives to surgery which may help with the symptoms caused by the hip problem. These include:
- Pain-relief medications – such as paracetamol
- Anti-inflammatory medications – these medications can be harmful if used long term and you should discuss the use of these medications with your doctor before starting
- Walking aids – such as walking sticks or frames
- Physiotherapy – exercises to improve muscle strength may help with mobility and reduce pain
- Weight loss – being over weight can make your hip pain worse. Loosing weight can help reduce pain and also lead to better results if you have the operation.
What are the benefits of hip replacement surgery
A hip joint replacement is usually a very succesful operation and will help to:
- Reduce pain
- Improve mobility: You should be able to move about more freely after your hip operation.
- Improve your quality of life: With less pain and better mobility, you be able to carry out your daily tasks more easily.
What can you expect to be able to do after a hip joint replacement?
It is important to understand what a hip replacement can and cannot do before deciding to have the operation.
After the hip replacement operation, most patients are able to return to gentle exercise such as:
- Walking
- Swimming
- Golfing
- Dancing
- Bike riding (gentle riding)
High impact sports are not recommended after a hip replacement. These activities can place too much stress on the hip and lead to early wear and tear of the hip replacement. High impact sports which are not recommended include:
- Running
- Football
- Basketball
- Martial arts
- Squash
- Water skiing / down hill skiing
What are the complications and risks of having a total hip replacement?
The complication rate following hip replacement surgery is very low. However like all surgery, there are risks that need to be considered when deciding to have hip replacement surgery.
Side effects
Side effects are symptoms that occur after every operation and are a normal part of the recovery from the operation. The main side effects which may last for several weeks after hip replacement surgery are:
- A sore hip
- Swelling and bruising around the thigh
Complications
Complications are uncommon problems that occur during or after the operation. Most people having hip surgery aren’t affected.
The general complications for all operations are:
- A reaction to the anaesthetic
- Infection of the wound or joint
- Excessive blood loss
- A blood clot, usually in a vein of the leg (known as a deep vein thrombosis or DVT)
Specific complications of hip replacement surgery are:
- Dislocation: Dislocation of the hip joint is when the ball of the hip pops out of the socket. Dislocation occurs in 1 – 4% of people who have had hip replacement surgery. A dislocated hip may be relocated without surgery or may require a new hip replacement to fix the problem.
- Infection: The hip replacement can become infected. This is a rare but serious complication of hip joint replacements. The risk of this occurring is between 0.02 – 1% of all people having a joint replacement.
- Fractures: A fracture is a break in the bone. Fractures can occur during a total hip replacement while the new hip is being put in place.
- Loose joint: The hip replacement may become ‘loose’. This is a rare complication that may require another operation to fix the problem.
- Nerve damage: Nerves can be damaged during the operation which can cause numbness or weakness in areas of the leg.
- Difference in leg length: After the operation, the leg that has been operated on may be slightly longer or shorter than the other side. This is the most common complication of hip replacement surgery. Usually it doesn’t cause any problems but may lead to pain or dislocation of the hip in some case.
It is important to note that the risks of certain complications may be higher or lower if the person having the operation has a medical condition that makes them more vulnerable to risks. For instance we know that obesity significantly increases the risk of an infection after a hip replacement.
The Operation
A hip joint replacement usually takes around two hours.
First, you will be given an anesthetic which puts you to sleep and relaxes your muscles to allow the operation to be performed safely and without any pain.
Your surgeon will make a cut (20 to 30 cm long) over your hip joint and then expose the ball and socket (hip joint). Some muscles may need to be moved out of the way or unattatched from the bone.
The damaged ball at the top of the thigh bone will be removed and replaced with an articifial ball which is inserted onto the end of the bone with a stem that is placed in the hollow centre of the bone.
The socket is then hollowed out and an artifical cup is put in place. The joint is then put back in place and the surrounding muscles reattatched.
Finally the skin is sewn back together using stitches or staples.
Hip revision surgery
During your original hip replacement, your hip joint was replaced with artificial hip parts. Hip revision surgery means having another operation to replace the worn out components of a hip replacement. Hip replacements usually last between 10 – 15 years.
Replacing an artificial hip joint is a more complex operation than the original hip replacement. It will often take longer and there are higher rates of complications than the original surgery.
What to expect before the surgery
Preadmission Clinic | Preparing for Surgery
Before your operation, you will be seen at the preadmission clinic to make sure you are fit for the operation and all the necessary tests are performed in preparation for the operation.
During the visit, you will be seen by a
- doctor
- nurse
- anaesthetist (if necessary)
Tests
Tests that may be ordered for you include:
- blood tests
- Xrays
- Hip and Pelvis
- Chest
- Urine Test
- ECG
Tips
Carry a list of your medications with you, including the name, dosage and how often you take it.
Medications
Our doctors will advise you which medications you should stop or can continue taking before surgery
Preparing Your Skin
Your skin should not have any infections or irritations before surgery. If either is present, contact your orthopaedic surgeon for a program to improve your skin before surgery.
Go see your dentist

Consider getting treatment for significant dental diseases (including tooth extractions and periodontal work) before your hip replacement surgery. Routine cleaning of your teeth should be delayed for several weeks after surgery. This reduces your chance of having an infection of your hip replacement.
Organise some help from your friends and family
Although you will be able to walk with crutches or a walker soon after surgery, you will need some help for several weeks with such tasks as cooking, shopping, bathing, and laundry.
If you live alone, your orthopaedic surgeon’s office, a social worker, or a discharge planner at the hospital can help you make advance arrangements to have someone assist you at your home. A short stay in an extended-care facility during your recovery after surgery also may be arranged.
Home Planning
The following is a list of home modifications that will make your return home easier during your recovery:
- Securely fastened safety bars or handrails in your shower or bath
- Secure handrails along all stairways
- A stable chair for your early recovery with a firm seat cushion (that allows your knees to remain lower than your hips), a firm back, and two arms
- A raised toilet seat
- A stable shower bench or chair for bathing
- A long-handled sponge and shower hose
- A dressing stick, a sock aid, and a long-handled shoe horn for putting on and taking off shoes and socks without excessively bending your new hip
- A reacher that will allow you to grab objects without excessive bending of your hips
- Firm pillows for your chairs, sofas, and car that enable you to sit with your knees lower than your hips
- Removal of all loose carpets and electrical cords from the areas where you walk in your home
The occupational therapist at the hospital will help to organise these things for you.
About the Operation

The right hip has a Total Hip Replacement and the left hip is normal.
Admission
Most people are admitted to hospital on the day of their surgery.
Anaesthesia
The anaesthetic team will see you and decide the type of anaesthetic that’s best for you.
The different types of anaesthesia include:
- General Anaesthetic. This type of anaesthetic puts you asleep during the whole procedure and a machine controls your breathing.
- Spinal Anaesthetic. An injection is placed into your back to numb your hip and legs. You will be awake during the procedure, however a sedative can be given to you to help you doze off.
- Nerve Blocks. This special injection is used to help with your pain after the operation and often used in conjunction with a general anaesthetic
What is the Hip Replacement made of?
Hip replacements are made of surgical grade metal (often chromium cobalt, stainless steel or titanium), highly wear resistant plastic or ceramic.
A hip joint is basically a ball and socket joint, and a hip replacement is designed to replace this normal anatomy.
A hip replacement is composed of a:
- Socket: It can be made of highly wear resistant plastic, metal or ceramic.
- Liner: The liner fits snugly into the socket to provide an ultra-smooth surface for the hip joint.
- Ball: The artificial ball component is smaller than your normal hip ball. It is incredibly polished and perfectly round and smooth. It is usually made of metal or ceramic.
- Stem: The stem fits snugly into your thigh bone (femur) to provide a stable structure for the ball. It is made of metal.
There are many types of hip replacements available, and your surgeon will decide which one is best for you.
Recovery Room
After the operation, you will be resting in the recovery room, where specially trained nurses will closely monitor you. This usually takes 1 to 2 hours. After which, you will be taken to your hospital room.
After the Operation 

Immediately after the operation
You will wake up in the recovery area after the operation is completed. You may not be able to feel or move your leg for the next few hours due to the anesthetic you have just had. You may need to have some painkillers after the anesthetic wears off, as the hip will be sore following the operation.
You may be given an injection to stop blood clots from forming in your legs. These injections are usually given on a daily basis whilst you are in hospital.
Day 1after surgery
You will have a blood test to check your blood levels and an X-ray to check the hip replacement is sitting correctly.
The wound will be checked and you will be given painkillers to manage the pain after the operation.
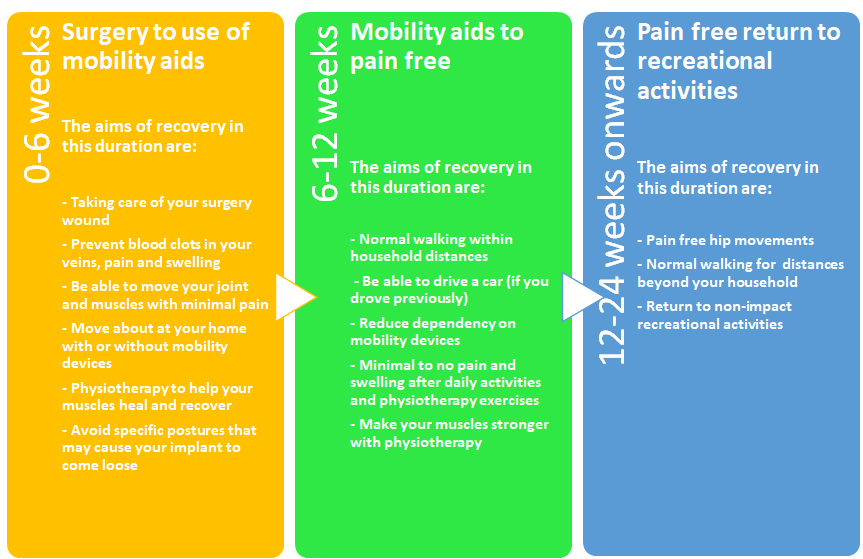
The physiotherapist will come to see you and give you simple exercises to start your recovery from the operation. With the physiotherapist, you will be able to walk with assistance of walking aids (crutches or frame) as early as the day of your operation.
During your hospital stay
Whilst in hospital you will be monitored to ensure there are no complications from your operation and that you are medically stable.
You will continue to see the physiotherapist on a daily basis who will prescribe exercises and help you to get back on your feet and walking. Often after the operation you may need a frame to walk with in the early phases of recovery and you will probably go home with crutches.
The physiotherapist, and your doctors will discuss with you whether you can go straight home after your hospital stay or whether you need to have some time with the rehabilitation team in the hospital.
Most people that are fit and well before their operation only stay in hospital for 4-5 days after their operation. If you have several other medical problems or you are slow to recover, your hospital stay may be longer.
Recovery and Rehabilitation
Wound Care
How do I look after my wound?
It is important to keep your wound as dry as possible.
Most patients are discharged home with a waterproof dressing, which can be left on for showering.
During the first 24 hours, it is normal to have some minor bleeding. After being discharded home, there should be no discharge, redness or bleeding around the wound.

If there is redness, discharge or a foul odor, please seek medical attention as soon as possible.
When will my stitches be removed?
There are a number of ways your wounds may be closed.
You may have either have
- nonabsorbable stitches
- absorbable stitches
- surgical staples.
The stitches or staples are usually removed 10-14 days after surgery.
Diet | What should I eat and drink?
There are usually no specific diet or extra vitamins / nutrients needed to recover from a total hip operation.
It is important to have a normal healthy balanced diet and plenty of nonalcoholic fluids.
Activity | What exercises should I do at home?
Physiotherapy and the exercises that you perform at home are extremely important to achieve the best results after a hip replacement.
After returning home, you should gradually be able to do more and more. It is important to look after your new hip and follow your surgeon’s and physiotherapy instructions.
Your program may include exerises that work on your:
- walking
- sitting
- stair climbing
- muscle strength
Avoiding Falls
A fall during the first few weeks after surgery can damage your new hip and may result in a need for more surgery.
Be careful on Stairs. Stairs are a particular hazard until your hip is strong and mobile, and you’ve regained your balance. You should use a walking aid such as cane, crutches, a walker. Use the handrails on your stairs or ask for someone to help you., or handrails or have someone help you.
Special Precautions
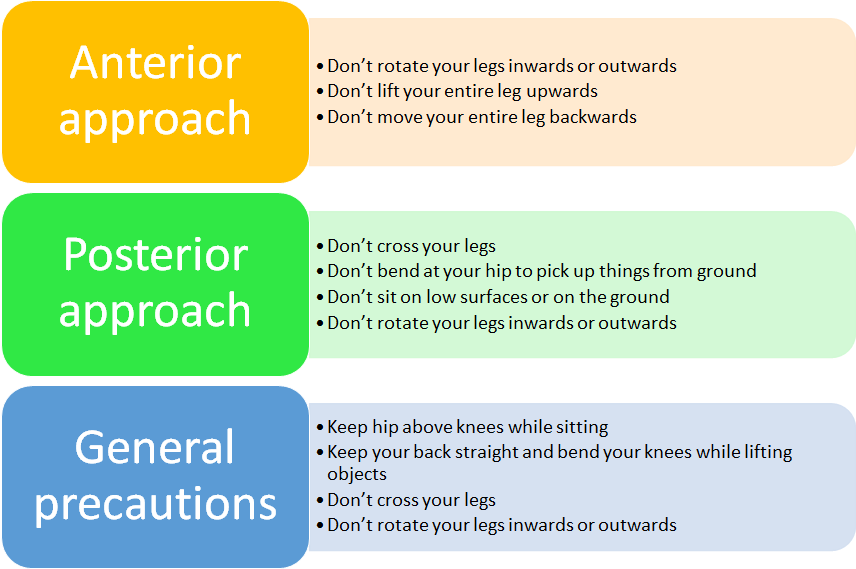
One of possible complications of hip replacement surgery is dislocation. Dislocation is most common during the first year after surgery, but can also occur at any time. There are certain positions and precautions that must be avoided.
- Do not sit or stand with your legs crossed.
- Do not bend your hips more than a right angle (90°).
- Do not turn your feet excessively inward or outward.
F.A.Q.s | Frequently Asked Questions
Anatomy | What is the hip joint?
The hip is one of the body’s largest weight-bearing joints. It consists of two main parts: a ball (femoral head) at the top of your thighbone (femur) that fits into a rounded socket (acetabulum) in your pelvis. Bands of tissue called ligaments (hip capsule) connect the ball to the socket and provide stability to the joint.
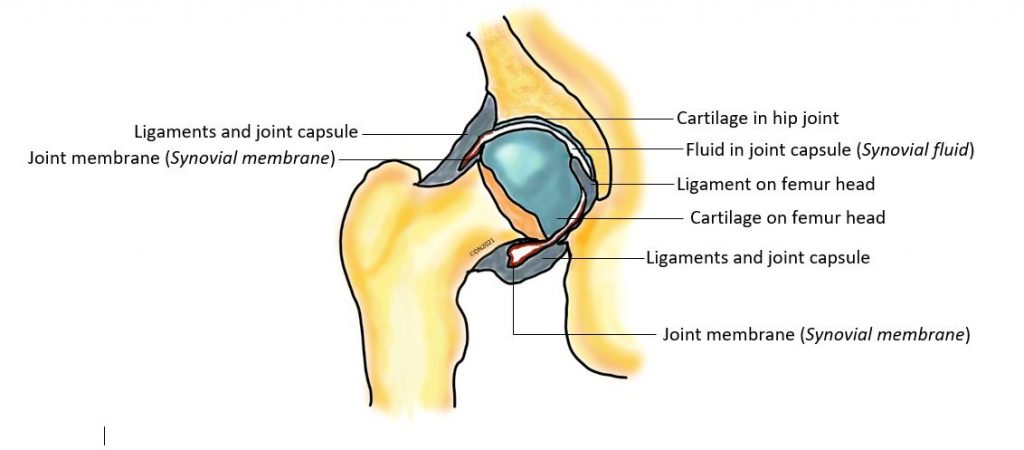
The bone surfaces of the ball and socket have a smooth durable cover of articular cartilage that cushions the ends of the bones and enables them to move easily.
A thin, smooth tissue called synovial membrane covers all remaining surfaces of the hip joint. In a healthy hip, this membrane makes a small amount of fluid that lubricates and almost eliminates friction in your hip joint (synovial fluid).
Normally, all of these parts of your hip work in harmony, allowing you to move easily and without pain.
Can I treat my hip pain without an operation?
Hip pain can be improved by many different methods.
These include:
- Medications. Such as paracetamol or anti-inflammatories.
- Changes to Activities. Modify the activities that cause you the pain.
- Walking aids. Such as a walking stick or cane can help off-load the weight on your painful hip and should be used on the opposite side to the painful hip. For example, if you have a painful right hip, you should use the walking stick in your left hand.
- Weight Loss. Losing weight can make you more mobile and help you with your symptoms.
- Modify your house. Modifications to your house may help you cope with your symptoms.
All these methods should be tried before considering an operation.
Will my hip replacement activate the metal detectors at airports?
Some hip replacements may activate metal detectors at airports and some buildings. Tell the airport personnel about your hip replacement if the alarm is activated.
How long will my hip replacement last?
Most hip replacements last 10 – 15 years and some may last as long as 20 years. It is important that you look after your hip replacement and avoid high impact activities such as running, jumping or contact sports.
How long does it take before I can walk after my hip replacement operation?
Most people walk the day after the operation or in the first 3 days following the operation. You will usually need to walk with a frame after the operation and often need crutches for the first two weeks following the operation.
Do I need to tell my dentist that I have a hip replacement?

It is good practice to tell your dentist that you have had a hip replacement. Currently, antibiotic prophylaxis for patients with prosthetic joints who are undergoing dental treatment is not routinely recommended in Australia. However, if you have immunodeficiency or your joint has been previously infected, your dentist will need to consult with your orthopaedic surgeon and GP, to decide on antibiotic requirement.
References
- An analysis of the risk of hip dislocation with a contemporary total joint registry. Khatod M, Barber T, Paxton E, Namba R, Fithian D. Clin Orthop Relat Res. 2006 Jun;447:19-23.
- Dislocation Following Total Hip Replacement: The Avon Orthopaedic Centre Experience. Ashley W Blom, Mark Rogers, Adrian H Taylor, Giles Pattison, Sarah Whitehouse, and Gordon C Bannister. Ann R Coll Surg Engl. 2008 November; 90(8): 658–662.
- Rates and outcomes of primary and revision total hip replacement in the United States medicare population. Mahomed NN, Barrett JA, Katz JN, et al. J Bone Joint Surg Am 2003;85:27.
- Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States medicare population. Katz JN, Losina E, Barrett J, et al. J Bone Joint Surg Am 2001;83:1622.
- Infection after total hip arthroplasty. The Avon experience. Blom AW, Taylor AH, Pattison G, et al. J Bone Joint Surg Br 2003;85:956.
- The importance of leg length discrepancy after total hip arthroplasty. A. Konyves,
- G. C. Bannister. J Bone Joint Surg Vol. 87-B, No. 2, Feb 2005
- Management of periprosthetic fractures: the hip. Berry DJ J Arthroplasty 17(4 Suppl 1):11–13. 2002
- Motor nerve palsy following primary total hip arthroplasty. J Bone Joint Surg Am. Farrell CM, Springer BD, Haidukewych GJ, Morrey BF. 2005;87(12):2619-2625.
- Total hip arthroplasty for primary osteoarthritis in patients fifty-five years of age or older. An analysis of the Finnish arthroplasty registry. Mäkelä KT, Eskelinen A, Pulkkinen P, Paavolainen P, Remes V. J Bone Joint Surg Am. 2008 Oct;90(10):2160-70.
- Exercise recommendations after total joint replacement: a review of the current literature and proposal of scientifically based guidelines. Kuster MS. Sports Med. 2002;32(7):433-45.
- Prophylaxis against pulmonary embolism in patients undergoing total hip arthroplasty. Khatod M, Inacio MC, Bini SA, Paxton EW. J Bone Joint Surg Am. 2011 Oct 5;93(19):1767-72.
- Antibiotic Expert Groups. Therapeutic Guidelines: antibiotic. Version 15. Melbourne: Therapeutic Guidelines Limited; 2014