Clubfoot is a common condition affecting just under 1 in every 1000 births in Australia. While most babies are born with some degree of ‘normal’ clubfoot, this is usually a temporary malposition that they will grow out of spontaneously.
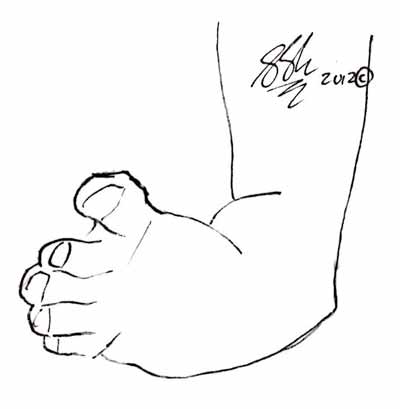
Babies with clubfoot have one or both feet twisted inwards (‘varus’) and down (‘equinus’). In most babies, this is simply due to the way the feet are ‘tucked up’ in the womb. In babies with clubfoot, the position of the feet is due to abnormalities in the joints, bones, tendons and other tissues in the foot. Paediatricians always check babies’ feet for clubbing after they are born, however it may not be possible to detect subtle clubfoot until later in life.
Clubfoot can range from mild and flexible to severe and rigid. Babies may struggle with walking and, in more severe cases, crawling. They may also develop sores on their feet.
Often, clubfoot can be detected by routine ultrasound scan while you are pregnant. In these cases, you will be able to discuss the implications of this with your doctor or an orthopaedic surgeon. There is no need to treat the baby until after the birth, however from then on there are many very effective treatments available.
Other Names for ClubFoot
- Talipes Equinovarus
- Talipes
Symptoms
The physical appearance of the foot may vary. One or both feet may be affected.
- The foot turns inward and downward at birth, and cannot be pulled straight.
- The calf muscle and the foot may be slightly smaller than normal.
- You may notice your child has deep folds in the skin on the inner surface of the ankle, and fewer if any skin creases on the outer surface.
Causes
The overall deformity of ‘clubfoot’ is due to a number of abnormalities in the structures in the feet. This can include:
- Navicular-talar subluxation. The navicular and talus are bones in the foot just below the ankle. In clubfoot, these two bones are slightly mal-positioned (subluxed), causing the foot to twist inwards.
- Tight and/or short posterior tibialis tendon and calcaneonavicular and calcaneofibular ligament. These structures support the position of the ankle and foot. When they are not correctly balanced they pull the foot out of position, causing it to twist inwards.
- Abnormal lower leg, ankle and foot muscles. Babies with clubfoot often have small or scarred muscles, in particular the gastrocnemius muscle (the large muscle you can feel on your calf) and Achilles tendon tends to be abnormal. This muscles tends to shorten more than normal, resulting in the foot pointing down.
- Abnormalities in the blood vessels. There are a number of large arteries that supply the foot. Babies with clubfoot tend to have fewer or smaller arteries. This most commonly affects the dorsalis pedis artery – the vessel that runs along the top of the foot.
It is unclear why all of these abnormalities occur. Sometimes there is a family history of clubfoot, suggesting that the disorder has been inherited, but many children with clubfoot have no apparent cause.
There are a number of syndromes that cause abnormal musculoskeletal development and are associated with clubfoot. Your orthopaedic surgeon and paediatrician will look for other signs of these syndromes, but it is important to remember that these are rare, and most babies with clubfeet do not have any other abnormalities.
Risk Factors
Some factors that are thought to play a part in the development of clubfoot include:
- Clubfoot tends to occur in male babies more often than in female
- A mother that smokes
- Family history of clubfoot
Investigations
The disorder is identified during a physical examination. A foot x-ray may also be done to check the position and shape of the bones.
Your doctor may also check your child’s spine and hips for other signs of musculoskeletal problems.
Complications
A number of secondary deformities may develop in the foot later in life. It is not always clear why these develop, but may be a combination of post-surgical overcorrection & intrinsic problems. These new deformities may include:
- Valgus Hindfoot -the heel tilts outward in relation to the leg.
- Calcaneus at increased angle – the heel is too vertical in relation to the leg.
- Flatfeet.
- Persistent rolling of the ankle (see Chronic Ankle Instability). In some cases, the foot may be correctly aligned but with a tendency to roll the ankle inwards. This can be corrected with surgery.
In some cases, residual clubfoot remains despite surgery, or re-develops later in life. This may require special footwear, extensive physiotherapy or extra surgery.
Treatment
Treatment for clubfoot is usually very effective, with little long-term impact on walking and running. Treatment will be more likely to succeed if it commences as early as possible, ideally shortly after birth. In the first months of life, your babies bones and tissues are quite soft and malleable.
There are a number of different treatments for clubfoot, and the method chosen for your child will depend on the type and severity of the clubfoot. In general, avenues for treatment will involve either physical therapy or surgery, and commonly a combination of the two.
The aims of treatment include:
- Allowing your child to walk and run normally
- Correcting the appearance of the foot
- Preventing the development of the other complications
Physical Therapy – Braces, tape, plaster casts and stretches.
There are a number of different programs used to correct clubfoot. This may involve:
A series of casts.
- The orthopaedic surgeon or paediatrician will move the foot into the correct position and then apply a plaster cast to keep it there. Gentle stretching and recasting occurs every week to improve the position of the foot. Generally, 5 to 10 casts are needed.
- The final cast remains in place for 3 weeks.After the foot is in the correct position, a special brace is worn nearly full-time for 3 months. After, it is used at night and during naps for up to 3 years.
Taping and stretching.
- An alternative method uses a combination of taping, stretches and exercise. Your paediatrician or orthopaedic surgeon stretches the legs and feet in special exercises every day for the first few months of life, and tapes the feet to hold them in place.
- After a few months, the exercises and stretches can be reduced to a few times a week and finally switched to more active method series of exercises as your child beings to crawl and walk.
- In this method, night splints are usually required for the first few years of life.
These physical measures are often very effective. Many children are able to walk and run normally long before kindergarten.
Surgery
There are two broad arms of surgery in clubfoot treatment. In many cases, a minor surgical procedure is used to supplement the ‘physical therapy’ of casts, braces etc. In other cases, more aggressive surgery is required.
Minor operations that may be used in conjunction with physical therapy include:
- Achilles tendon release. Many babies with clubfoot have a tight, short Achilles tendon. By lengthening this tendon, the foot is able to come back into neutral position.
More aggressive surgery includes fusion procedures like triple arthrodesis. This surgery involves correcting the position of the foot then fusing it in place. Only in the most severe cases of clubfoot will your surgeon consider fusion surgery, and this will only be in later life when the foot has stopped growing.
Follow-up Over Life
Most children who have been treated for clubfoot deformity will need long-term followup by a doctor until the foot has finished growing. This is to check the bones and tendons have grown normally and the clubfoot is not going to recur.
Seeking Advice
The paediatricians who assess your child at birth and the nurses who see you in early life will look specifically for signs of clubfoot. You can discuss any concerns you have with them.
If you notice your child is limping, or you think your child’s feet look abnormal see your family doctor.
Your Family Doctor (GP)
Your Family Doctor will be able to diagnose and help treat your problem. He or she will be able to
- tell you about your problem
- advise you of the best treatment methods
- prescribe you medications
- and if necessary, refer you to Specialists (Consultants) for further treatment
When to Contact a Medical Professional
If your child is being treated for clubfoot, see your GP if:
- There are problems with the cast/brace – for example it slips off or starts to cause unbearable irritation.
- You notice swelling, bleeding, or a change in colour of the toes beneath the cast
- If the toes can no longer be seen
Longterm, you should regularly check your child’s feet. It is often easiest to do this when you’re buying new shoes for your growing child. Check that the feet are still aligned well and do not have any ulcers or callouses that might indicate they are rubbing against their shoes.
Prevention
It’s not possible to prevent clubfoot in your child.
F.A.Q. | Frequently Asked Questions
Isn’t my child too young for surgery? What are the risks?
Perhaps surprisingly, many children tolerate surgery very well, better than many adults.
Does my child have other abnormalities?
Usually, no. Your doctor will check your child’s spine, hips, legs and other joints but most children with clubfoot are fine.
Outlook (Prognosis)
The outcome is usually good with treatment.
