What is an Ankle Replacement?
An Ankle Replacement, also called a Total Ankle Replacement or Total Ankle Arthroplasty, is an operation where the joint structures are replaced by plastic and metal components.
The surfaces of the bones in the ankle joint (the tibia and talus) are polished then plated with metal fittings. A plastic surgical bearing is then placed between the metal to cushion the surfaces against one another.
The most common reason for needing an Ankle Replacement is severe osteoarthritis. The operation takes about two hours and is usually performed under general anaesthesia.
Ankle replacement preserves the movement of the ankle joint and relieves pain. This allows for a more normal walking pattern and reduces the risk of secondary arthritis in the joints around the ankle. Ankle arthrodesis is an alternative to ankle replacement.
It takes weeks to months to recover from an ankle replacement, and during this time physiotherapy rehabilitation is required.
Diagram of an Ankle looking from the front. It shows an Ankle with Arthritis
Who is this operation for?
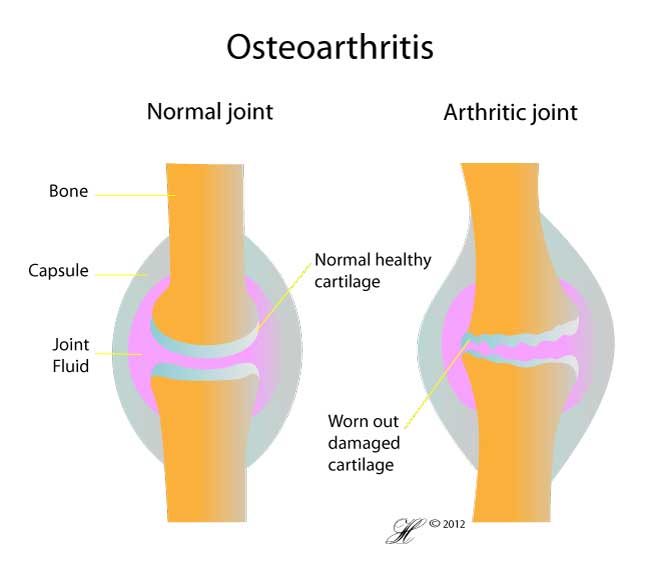
Diagram of a normal joint and a joint affected by osteoarthritis
The Total Ankle Replacement is considered for patients with arthritis of the ankle in whom non-operative treatment has been exhausted. This is usually osteoarthritis or inflammatory arthritis like rheumatoid arthritis.
Occasionally ankle replacement is considered to fix injured ankles where other surgery has failed.
When do I need a total replacement?
Usually your GP will refer you to an orthopaedic surgeon, who will discuss when a replacement is appropriate. Usually, you will have:
- Severe pain and disability
- Reduced quality of life
- Inadequate symptom relief from medications
When these conditions are met, your surgeon will discuss the relative advantages and disadvantages of a total replacement against the alternative fusion operation (see Ankle Arthrodesis).
Fusion vs Replacement
There are a number of factors that can cause you to choose one method over another, and you should discuss the following with your surgeon:
- Your expected level of activity post-operation. In general, fused bones withstand greater stress than the hardware used to replace the ankle. For this reason, many surgeons will tend to perform a fusion operation in younger people with increased demands on their ankle.
- The health of other joints in your foot. As fusion tends to put increased strain on the other joints in your foot, poor movement or pain in other joints may make a replacement more appropriate.
Another point to keep in mind is that some forms of ankle replacement can be converted into a fused ankle if complications occur. In contrast, an ankle that fails to fuse cannot be replaced.
Contraindications
This surgery cannot be performed when you:
- Have a general infection or an infection in the foot
- Have a very unstable ankle
- Have diabetic deformity
- The key bone connecting your foot and lower leg (the talus) is either very weak (osteoporosis), infected (osteomyelitis) or dead (osteonecrosis)
In these situations, you may still be eligible for arthrodesis.
What are the complications?
Are there any risks associated with a Total Ankle Replacement?
Some complications include:
- Short term swelling and longterm stiffness of foot and ankle
- Bleeding & infection— All invasive procedures carry a small risk of infection and blood loss.
- Delayed wound healing.
- A joint that continues to be painful.
- Need for further surgery. This can be due to:
- Malpositioning of the joint.
- Irritation or infection of the hardware.
- ‘Failure’ – it’s important to remember that ankle replacements wear out over time and will eventually need to be replaced. Around 90% of ankle replacements last 5 years, and approximately 75% last ten years.
- Injury to nerves – Numbness or tingling can occur at the wound or in the foot. This is usually temporary but sometimes may be permanent.
- The nerve most at risk during an ankle replacement is the deep peroneal nerve which supplies a small area of skin between the toes.
- Blood clots— Deep vein thrombosis (DVT) or pulmonary embolism (PE) is rare. If you or your family have a history please let us know.
- Numbness, tingling or irritation of the leg – during the operation your surgeon will place a tight bandage (tourniquet) around your thigh to reduce blood loss. This can cause temporary discomfort after the operation.
For more information on the general risks of surgery, see Complications of Surgery.
Before the operation
Preadmission Clinic | Preparing for Surgery
Before your operation, you will be seen at the Preadmission clinic to make sure you are fit for the operation and all the necessary tests are performed in preparation for the operation.
During the visit, you will be seen by a
- doctor
- nurse
- anaesthetist (if necessary)
If you have chronic lung or heart disease, diabetes or other risk factors for complications during surgery, you may require a detailed anaesthetic assessment.
Tests
Tests that may be ordered for you include:
- blood tests
- X-ray of ankle and/or foot. Sometimes, your surgeon may request X-Rays of your other ankle to have a comparison.
- Xray of your Chest
- Urine Test
- ECG
Preparing Your Skin
Your skin should not have any infections or irritations before surgery. If either is present, contact your orthopaedic surgeon for a program to improve your skin before surgery.
Tip
Carry a list of your medications with you including the name, dosage and how often you take it.
Medications
Our doctors will advise you which medications you should stop or can continue taking before surgery. Please make sure you inform your doctors if you are taking any blood thinning medications, like warfarin or aspirin.
If you have rheumatoid arthritis, you may need to speak with your rheumatologist about which drugs are safe for surgery.
What happens during the operation?
Ankle replacements can take 1-3 hours to perform. When you are brought to the operating theatre, your surgeon, anaesthetist and theatre nurse will meet you. your surgeon will perform a quick assessment of your foot then draw lines on your ankle to mark out important structures that need to be avoided. After this, your anaesthetist will put you to sleep (general anaesthetic, or regional/spinal anaesthetic with sedation).
Once in theatre and asleep, your surgeon will prep you for the operation. This usually includes:
- A regional anaesthetic to numb pain from the area.
- Applying a tight bandage (tourniquet) to the thigh to reduce bleeding
- Positioning the leg and ankle.
- Sterilising the skin over and around the ankle.
When this is done, your surgeon can make a cut to reach the ankle joint. The position and length of the incision will vary depending on the type of prosthetic joint being used. Commonly, the incision will about 10cm long and on the front of your ankle joint.
Once the cut has been made, your surgeon can carefully separate the muscles and ligaments beneath the skin to reach the joint. The ligaments and capsule around the joint are then divided to expose the bone.
Your surgeon will then place equipment into the joint that will separate and cut the bones. When this is complete, your surgeon will carefully position the implant before fixing it in place.
After this, the tissues around your joint will be pulled back into position and stitched together before your skin is closed.
What happens after the operation?
When you awake from surgery, you will be in the recovery room with a plaster on your leg. At this point, you should feel little if any pain as the anaesthetic injected into your leg by your surgeon will still be working.
Once you are awake, you will be returned to the wards and kept in hospital for 2-3 days. During this time you will need to keep your leg elevated nearly all the time.
Before you can be discharged, physiotherapists will show you how to move around using crutches and without putting any weight on your foot. You should remain non-weight-bearing for the first few weeks after your operation, and can only begin using your leg once an X-Ray has confirmed your bones are healing.
Your cast will need to be assessed and changed at 10-14 days after your surgery (see Caring for your Cast). At this first follow-up appointment your surgeon will inspect your ankle and get X-Rays to confirm the implant is correctly positioned and your bones are healing well. Your stitches may also be taken out at this point.
To control swelling and help your ankle to heal, keep your leg elevated as much as possible in the first week after surgery by sleeping with your foot raised on pillows and sitting with your leg resting up on a chair.
Recovery and Rehabilitation
What happens after discharge?
We will arrange to see you in the Orthopaedic Outpatients’ Department two weeks following the surgery. The back slab will be removed and your wound will be inspected. If the wounds are healed then a removable boot will be applied for you to walk in. This is to be worn during the day for walking but need not be worn at night. With this boot on, you can begin to take weight through your ankle 2 weeks after your operation. You will need this boot until you are 6 weeks after your operation. During this time it is likely that you will continue to require the use of your crutches. After the backslab has been removed, we will send you to see a Physiotherapist as an Outpatient. They will give you exercises to move your ankle and teach you to walk with your removable boot.
When can I return to work?
If you have an office type of job and you are able to elevate the leg then you may return to work approximately 4 weeks following surgery. However, if your job is physically demanding and usually involves long periods on your feet then it is advisable not to return for up to 3 to 6 months. This decision will depend on where your type of employment falls between these two extremes.
When is it safe to drive?
If you have a replacement on the left ankle and an automatic car, you can usually drive by two to four weeks after your operation. Otherwise, it will take you about 2 to 3 months to drive with your replaced ankle. You must be able to perform an emergency stop. Your insurance company must be notified regarding the type of operation that you have undergone to ensure that cover is valid.
What should I do if I have a problem?
If you experience severe pain, excessive swelling, discharge, excessive numbness or pins and needles please report it to your GP. If you cannot contact your GP you should visit the Emergency Department as quickly as possible.
F.A.Q.s | Frequently Asked Questions
References
Briggs, T., et al., ‘Operative Orthopaedics: The Stanmore Guide’, Hodder Arnold Ltd., UK, 2010.
Chou, L. B., et al., ‘Osteoarthritis of the Ankle: The Role of Arthroplasty’, Journal of the American Academy of Orthopaedic Surgeons, Vol. 16, No. 5, May 2008, pp. 249-259.
Easley, M. E., ‘Perspectives on Modern Orthopaedics: Total Ankle Arthroplasty’, Journal of the American Academy for Orthopaedic Surgery, Vol. 10, No. 3, May/June, pp 157-167.
