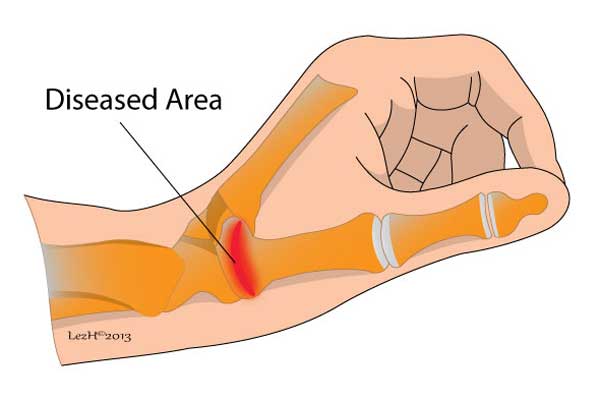
Arthritis of the thumb, also called basal joint arthritis, occurs when there is irritation and destruction at the base of the thumb. This is most commonly due to osteoarthritis – ‘’wear and tear’’ arthritis.
Osteoarthritis at the base of the thumb is more common in women than men, and usually occurs after the age of 40. Having arthritis of the thumb can lead to pain, swelling, stiffness and difficulty in performing daily activities.
Symptoms
The symptoms associated with arthritis of the thumb, include:
- Pain or discomfort at the base of the thumb. This is often aggravated by activities such as gripping, grasping, pinching an object between thumb and forefinger, opening a door and snapping your fingers.
- Swelling and stiffness at the base of thumb.
- An aching discomfort after prolonged use of thumb.
- Limited or decreased range of motion.
- Reduced strength in gripping or grasping object.
- Deformity: Enlarged and out-of joint appearance of the joint at the base of the thumb.
As the condition progresses, you may even experience pain when resting or not using your thumb.
Causes
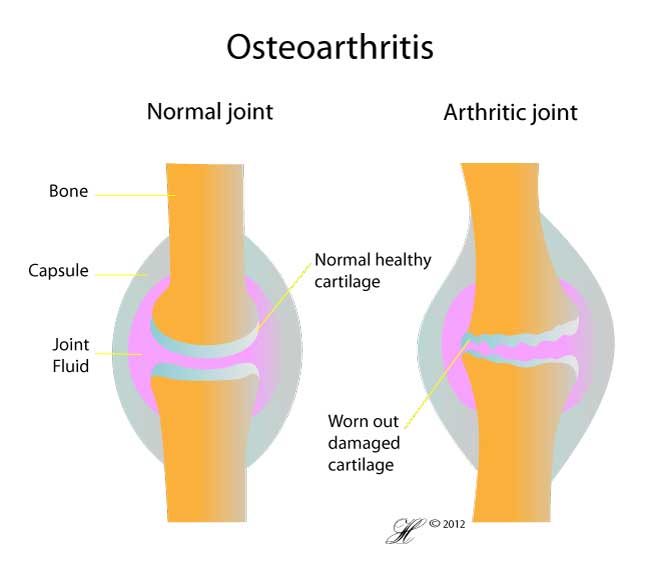
The exact cause of thumb arthritis, as with osteoarthritis in general is not known. In a normal joint, the cartilage covers the end of the bone and serves as a shock absorber to provide smooth and friction-free movement. With thumb arthritis, the cartilage wears out and smooth surface roughens. The bones then rub against each other, producing joint damage and friction.
The proposed causes include being overweight, joint injury and stress, hereditary, muscle weakness and repetitive usage of the joint. It is usually the combination of all these factors which lead to the development of thumb arthritis.
Risk Factors
The risk factors include:
- Female, age more than 40.
- Previous trauma or injury such as, sprain or fracture to the base of the thumb.
- Hereditary: Malformed joint and laxity of the ligaments.
- Certain conditions which alter the function and structure of cartilage, such as rheumatoid arthritis.
- Activities that place high stress on this joint.
Investigations
Your doctor may perform a history taking and physical examination.
History: Your doctor will ask you about your symptoms, pain characteristics and pattern, any specific or previous injuries to your thumb.
Physical Examination: Your doctor may apply pressure at the base of the thumb to elicit any pain or discomfort. He or she will also be looking for any swelling, lumps and assessing the range of movements of the thumb. If the movement of your thumb produces a grinding sound (crepitus) and pain, this indicates that the cartilage has worn out and bones are directly rubbing each other.
An x-ray may show deterioration of the joint itself, loss of joint space and any other structural changes such as bony spurs or calcium deposits. Symptom severity often does not correlate with x-ray findings.
Your doctor may recommend other imaging scans such as, CT scan, MRI and bone scan.
Complications
As the condition progresses, there will be increased pain, stiffness and reduced mobility of the thumb. This can significantly affects the simplest acts of daily life, such as buttoning a shirt, using utensils or turning a key.
Treatment
Treatment of thumb arthritis is to reduce discomfort or pain, improve joint movement and reduce disability. Your doctor may recommend a variety of treatment options. In the early stages, arthritis at the base of the thumb will respond to non-surgical treatment.
Non – surgical:
- Brace or Splint: Your doctor may recommend a brace or splint to support the thumb. Several types of splints are available. These devices help to reduce pain and prevent thumb deformity from getting worse. A thumb stabiliser is a type of thumb splint that is made from heat-mouldable plastic. Depending on your needs, you may wear the splint during the night, when the disease flares up or throughout day and night.
- Medication: Anti – inflammatory medications such as over the counter medications (OTC) – aspirin, ibuprofen or naproxen may reduce the swelling and inflammation around the joint. Long term usage of these drugs can lead to gastric ulcers, gastrointestinal bleeding, liver and kidney damage.
- Steroids: Your doctor may inject steroids into the basal joint, but this only gives temporary relief which lasts from several weeks to months. When steroid injection(s) is combined with splinting, this is shown to be more beneficial and successful than steroid injection(s) alone.
If the condition worsens, and do not respond to the non – surgical treatments, your doctor may then recommend surgical treatments.
Surgical: Each of the following procedures can be done on an outpatient basis.
- Arthrodesis (joint fusion): Your surgeon permanently fuses the bone together in the affected area. This will reduce pain and increase stability. This is quite often done in younger people who need a stronger grip or pinch than they need the fine motion of the thumb. Individuals who use their hand for heavy work will prefer this method rather than arthroplasty.
- Arthroplasty (joint replacement): Your surgeon replaces the affected area with a graft from one of your tendons. Plastic or metal prosthesis can also be used. The prosthesis acts as a spacer to fill the gap created when the arthritic surfaces of the 2 bones are removed.
- Trapeziectomy: Trapezium bone, which is just next to the base of the thumb is removed.
- Osteotomy: Bone cutting – your surgeon repositions the bone to correct any deformities. This can reduce or eliminate pain.
Seeking Advice
Your Family Doctor (GP)
Your Family Doctor will be able to diagnose and help treat your problem. He or she will be able to
- tell you about your problem
- advise you of the best treatment methods
- prescribe you medications
- and if necessary, refer you to Specialists (Consultants) for further treatment
Prevention
Don’t pinch and clutch: You need to avoid pinching items, such as clutch purse, get yourself a shoulder bag or an arm strap. Hold a mug in the palm or palms of your hand, instead of griping the handle of the mug.
Exercise your hands: Give them a good stretch. Massage your thumb and fingers. Exercise that move your thumb through its full range of motion can help improve your joint’s mobility.
Pay attention to what you are doing: We use our hands all the time in our daily activities and this can’t be avoided. However, if you are putting excessive stress on your joints, this will result in pain. Think about better ways to perform these activities, which are kinder and gentler to your hands or thumb.Take daily supplements: Take daily supplements that contain chondroitin sulphate, glucosamine, vitamin C and D, as these will strengthen your joints.
F.A.Q. | Frequently Asked Questions
What happens after surgery?
Your post-operative recovery depends on the type of surgery you had. Open surgery requires a longer recovery period than a less invasive method such as arthroscopy. Your hand will be bandaged with a thumb splint and a well – padded dressing after joint replacement, arthroscopy or ligament construction surgery. With joint fusion surgery, the thumb is placed in a cast to immobilise the joint for about 3 months.
Rehabilitation
A rehabilitation program, often involving a physical therapist and occupational therapist, helps you to strengthen and stabilise the muscles around the thumb. You may need these sessions for up to 8 weeks. Other exercises involve improving dexterity and motor control of your hand. Most patients are able to resume their normal daily activities and they are quite satisfied with the results.
