Sacroiliitis is an inflammation of one or both of the sacroiliac joints, which connect your lower spine and pelvis. With sacroiliitis, even the slightest movements of your spine can be extremely uncomfortable or painful for you.
Sacroiliitis can be difficult to diagnose, and it may be mistaken for other causes of low back pain, including sciatica, herniated disks and strained muscles. Sacroiliitis may be associated with a group of diseases called spondyloarthropathies, which cause inflammatory arthritis of the spine.
Treatment for sacroiliitis may involve a combination of you resting, receiving physiotherapy and taking medications.
Symptoms
Sacroiliitis symptoms may include:
- Pain and stiffness in your lower back, thighs or buttocks
- Pain that worsens with walking because the motion of your hips strains your sacroiliac joints
- Inflammation in one or both of your eyes (uveitis or iritis)
- Psoriasis, an inflammatory skin condition
- Pain radiating down your leg
- Limping
- Decreased range of motion in your lower back
- A fever that appears quickly
Causes
A wide range of factors or events may cause sacroiliitis:
- A traumatic injury or sudden impact, such as a motor vehicle accident or a fall, affecting your spine, lower back, pelvis or buttocks.
- Spondyloarthropathies, which include ankylosing spondylitis, arthritis associated with psoriasis and others.
- Degenerative arthritis, also called osteoarthritis of the spine, causing degeneration of the sacroiliac joints, which can cause mild inflammation and pain.
- Pregnancy, because the pelvis must stretch to accommodate childbirth.
- Infection of the sacroiliac joint, which may result from a number of infections.
Risk Factors
The following factors may increase your likelihood of getting the condition:
- A history of bone, joint or skin infections. Some people are more prone to infections, and an infection is one possible cause of sacroiliitis.
- Injury or trauma to your spine, pelvis or buttocks. Torn ligaments or trauma may create inflammation or infection of the sacroiliac joints.
- Urinary tract infection. This infection may spread from your urinary tract, which includes your kidneys, bladder and urethra, to your sacroiliac joints.
- Pregnancy. The pelvic bone’s expansion to prepare for childbirth may inflame the area around your sacroiliac joints.
- Endocarditis. This infection of your heart’s inner lining may spread to your sacroiliac joints.
- Illicit drug use. People who inject drugs may have a higher risk of developing sacroiliitis.
Investigations
Screening and diagnosis of sacroiliitis is difficult, but your doctor may confirm a diagnosis based on:
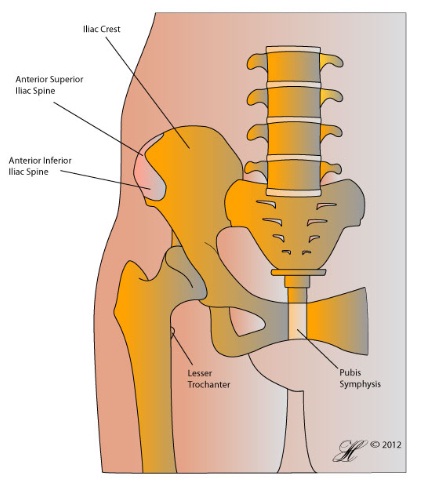
- Localized pain that seems to be on or around your sacroiliac joints, which a doctor can determine by pressing on your sacroiliac region while you move in certain ways to gently stress the sacroiliac joint.
- X-rays of your sacroiliac joints
- CT scan or magnetic resonance imaging (MRI) scan of your sacroiliac joints
- Cultures of fluid from the sacroiliac joint
- Blood culture, if the cause appears to be an infection
Complications
Delayed treatment of sacroiliitis — either because of an incorrect diagnosis or because you’ve put off going to your doctor — can cause serious harm to your sacroiliac joints.
Sacroiliitis may be part of a larger inflammatory arthritis condition known as ankylosing spondylitis. Complications of this condition can be very serious, including difficulty breathing, spine deformities, lung infections and heart problems.
Treatment
The type of treatment your doctor will recommend depends on the signs and symptoms you’re having, as well as the underlying cause of your sacroiliitis.
Medications
Medications used for sacroiliitis treatment may include:
Nonsteroidal anti-inflammatory drugs (NSAIDs). These pain-relieving drugs reduce swelling and inflammation. NSAIDs include indomethacin (Indocin) and naproxen (Aleve, Anaprox, others). Your doctor may prescribe these medications on an as-needed basis or continuously, depending on the severity of your condition.
Taking NSAIDs can lead to side effects, such as indigestion and stomach bleeding. Other potential side effects may include damage to your liver and kidneys, and high blood pressure. Except for aspirin, NSAIDs may also increase your risk of cardiovascular events, such as heart attack or stroke. The risk of side effects from these medications is higher in people who already have pre-existing medical conditions, such as liver or heart disease.
Corticosteroids. These medications, such as prednisone and methylprednisolone (Medrol), reduce inflammation and pain and slow joint damage. Cortisone injections can be used for localized pain relief that lasts a period of months.
In the short term, corticosteroids can make you feel dramatically better. But when used for long periods of time, they may cause serious side effects. Side effects may include an increased risk of infection, easy bruising, thinning of bones, cataracts, weight gain and a round face. Doctors often prescribe a corticosteroid to relieve acute symptoms, with the goal of gradually tapering off the medication.
For people with sacroiliitis associated with ankylosing spondylitis, there is no definitive evidence that oral steroids will help, and people with ankylosing spondylitis are more prone to developing osteoporosis.
Disease-modifying anti-rheumatic drugs (DMARDs). These medications include sulfasalazine and methotrexate . Doctors prescribe DMARDs to limit joint damage. Taking these drugs at early stages in the development of a joint condition is especially important to slow the disease and save the joints and other tissues from permanent damage.
Because many of these drugs act slowly, DMARDs typically are used with an NSAID or a corticosteroid. While the NSAID or corticosteroid handles your immediate symptoms and limits inflammation, the DMARD modifies the disease itself. Sulfasalazine may be helpful in treating arthritis of the leg and arm joints, but it’s currently not considered effective for people with the spinal symptoms associated with ankylosing spondylitis. Studies done on another drug, methotrexate, have had conflicting results. More studies are needed to determine whether methotrexate will be useful in treating sacroiliitis related to ankylosing spondylitis.
Tumor necrosis factor (TNF) inhibitors. These therapies, which include etanercept (Enbrel), adalimumab (Humira) and infliximab (Remicade), block a cell protein (cytokine) that acts as an inflammatory agent. Blocking the TNF cytokine may help reduce pain, stiffness, and tender or swollen joints. Because of their high cost, these medications are generally considered only after you’ve tried other treatments for at least three months without success.
Physiotherapy
Treatment for sacroiliitis may also involve physiotherapy and rest to help manage pain and stiffness. Your doctor or physiotherapist can help you learn range-of-motion and stretching exercises to maintain joint flexibility, and strengthening exercises to give your muscles additional stability.
Looking After Yourself
These actions you can take on your own may help:
- Don’t smoke. Smoking decreases blood flow to the infected area and makes it harder for your body to fight disease.
- Medications. Keep up with any prescribed medications. Medications are the most effective when taken routinely and appropriately, as prescribed.
- Physiotherapy. Follow through with physiotherapy exercises and rest. Both are crucial to maintaining joint mobility and recovering fully.
Seeking Advice
Your Family Doctor (GP)
Your Family Doctor will be able to diagnose and help treat your problem. He or she will be able to
- tell you about your problem
- advise you of the best treatment methods
- prescribe you medications
- and if necessary, refer you to Specialists (Consultants) for further treatment
You’re likely to start by first seeing your family doctor or general practitioner. However, because sacroiliitis can be difficult to diagnose, you may be referred to a rheumatologist or an orthopaedic surgeon.
This condition is sometimes hard to diagnose because thick muscle tissue surrounds the sacroiliac joints, so their location deep in the muscles of your buttocks makes these joints hard to examine. What’s worse is that the pain may be so severe that you can’t or don’t want to move much during the screening process, making it harder for your doctor to pinpoint the pain. Additionally, diagnosis is difficult because the signs and symptoms of sacroiliitis are similar to many other causes of low back pain.
Because appointments can be brief, it’s a good idea to be well prepared for your appointment.
Bring along information about yourself
It can be a great help for your doctor if you bring along the following information about yourself
- A list of your medications, including the name and dosage.
- Information about your medical problems and past treatment
- Previous investigation results, such as xrays and blood tests.
Prepare a list of questions for your doctor
- Write down any symptoms you’re experiencing, including any that may seem unrelated to the reason for which you’re scheduling your appointment. For example, people with sacroiliitis may have eye inflammation in addition to lower back pain.
- Write down key personal information, including any major stresses or recent life changes. Knowing that you were in a car accident or had a major fall recently could help your doctor make the diagnosis.
- Write down any questions you have, because it can be hard to remember to ask everything.
Some basic questions to ask include:
- What is the likely cause of my symptoms?
- Are there any other possible causes for these symptoms?
- What kinds of tests will I need?
- What types of treatments are available for sacroiliitis?
- What kinds of side effects does each type of medicine have?
- Is there anything I can do on my own to help improve my symptoms?
- Do I need to see a specialist?
- How long will it take before I begin to feel better?
What to expect from your doctor
Your doctor will likely ask you a number of questions, such as:
- When did you first begin to experience symptoms?
- Did anything unusual precede the pain, such as an illness, car accident or a fall?
- Are your symptoms continuous, or do they come and go?
- How severe is the pain?
- Do any activities worsen your symptoms?
- Does anything make you feel better?
- Have you ever had problems taking any medications?
What you can do in the meantime
As you wait for your doctor’s appointment, you can take nonsteroidal anti-inflammatory drugs (NSAIDs) to ease your pain. However, if you have pre-existing cardiovascular disease, kidney disease or liver problems or have had gastrointestinal bleeding, check with your doctor before taking these medications.
Prevention
In order to prevent sacroiliitis that is caused by an inflammatory arthritis condition such as psoriatic arthritis, early diagnosis and treatment should be sought from your medical practitioner. If the condition is diagnosed and treated before sacroiliitis has set in, there is a chance that this condition may be avoided.
Avoiding traumatic injuries such as falls or car accidents will avoid a traumatically induced sacroiliitis.
In pregnancy, sacroiliitis may be avoided by ensuring the muscles of the pelvis and lower back are strong. This can be seen to by a physiotherapist that is specialised in exercise therapy.
