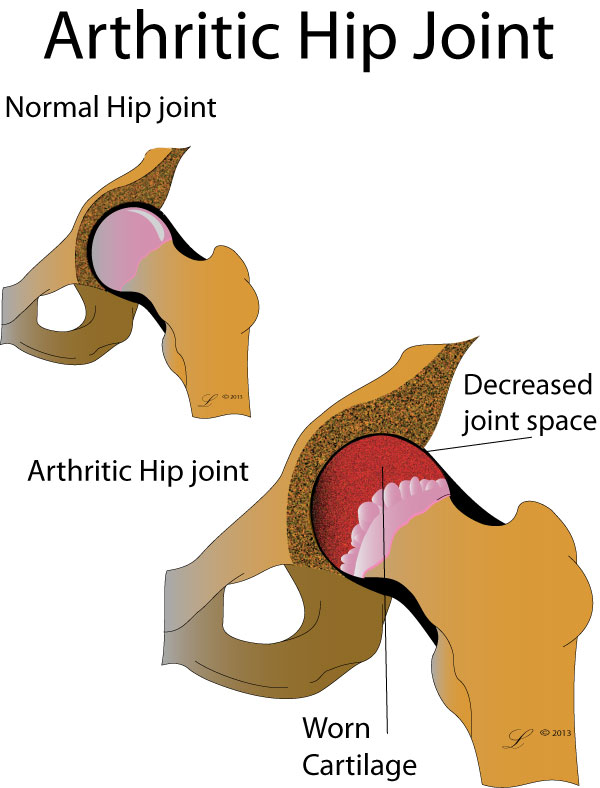
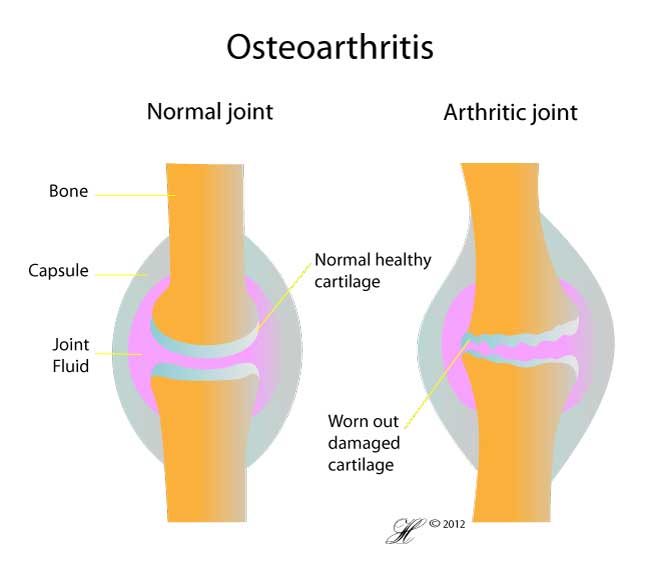
Your hip joint is covered by a smooth and glistening covering called articular cartilage. This cartilage helps your hip move and glide smoothly.
Over time, your articular cartilage can wear away. This is called osteoarthritis and is often referred to as ‘wear and tear’. Over time, the cartilage can break down so much that it no longer cushions the bones.
As well as cartilage break down, bone spurs can form in osteoarthritis which may limit the movement of the joint. This can lead to a stiff and painful hip.
Symptoms
The symptoms of osteoarthritis include:
- Stiffness
- Joint pain
- Muscle weakness
The pain may be felt in the groin, buttock or front of the thigh. It may be worse first thing in the morning but get better with movement and then get worse again towards the end of the day. It is often better with rest.
You may lose the ability to bend or straighten the hip. If the pain is bad enough to limit your movement then the muscles of the hip can become weak.
Causes
You may be at a greater risk of developing osteoarthritis if:
- You have a family history of the disease
- If you are elderly or overweight, then you also have a greater risk of getting hip osteoarthritis
- You may be at greater risk if you have participated in weight-bearing sports (e.g., running at an elite level), or occupations that require prolonged standing, lifting, or moving of heavy objects
It is important to remember that even if you don’t have these risk factors, you can still develop osteoarthritis.
Investigations
The first step of diagnosis is seeing your doctor who will take a medical history. Following this your doctor will examine your hip. This may involve bending the hip up and down as well as other movements to check for pain or a reduction in the amount of movement in the hip.
Your doctor may then send you for an X-ray which can show the signs of osteoarthritis such as bone spurs or wearing out of the joint.

Sometimes, a CT scan or an MRI is needed to rule out other causes of hip pain such as:
Treatment
Unfortunately there is no treatment that can reverse the process of osteoarthritis. Once the cartilage has worn away, it can not be replaced. However there are several treatment options which can help to reduce pain, maintain hip mobility and reduce the limitations on daily living.
Treatment options are often divided into non-surgical and surgical.
Non surgical options
- Exercise. A program of gentle, regular exercise such as cycling, swimming or water aerobics can help to keep your joint moving and improve strength of the surrounding muscles.
- Physiotherapy can help with improving hip mobility. Physiotherapists can also help with developing an exercise program which is suitable for the varying degrees of hip osteoarthritis.
- Weight loss (if overweight) can help to reduce the symptoms of hip osteoarthritis.
- Walking aids. The aid of a walking stick held in the opposite hand to the problematic hip can significantly improve the symptoms of osteoarthritis felt whilst walking.
- Assistive devices such as hand rails in the bathroom can help with activities of daily living.
- Pain medication can be of benefit in hip osteoarthritis. Paracetamol is the first line of pain medication and has been shown to be effective in relieving the pain caused by osteoarthritis. Other non-steroidal anti-inflammatories may also be helpful but you should consult your doctor in order to discuss their suitability for you.
Surgical options
If your hip osteoarthritis becomes severe, surgery may be necessary to improve the hip mobility and the level of pain. Operations include:
- total hip replacement (also called hip arthroplasty, THR)
- hip arthroscopy
Alternative medicine
Glucosamine and fish oils are often recommended as being helpful in improving symptoms of osteoarthritis. There have been studies carried out on these supplements and unfortunately they have found to be of little benefit.
Often these treatments are expensive, but not necessarily very beneficial. Always talk to your doctor before starting an alternative therapy for your hip condition.
Seeking Advice
Your Family Doctor (GP)
Your Family Doctor will be able to diagnose and help treat your hip problem. He or she will be able to
- tell you about your problem
- advise you of the best treatment methods
- prescribe you medications
- and if necessary, refer you to Specialists (Consultants) for further treatment
Your Orthopaedic Surgeon
Your Orthopaedic surgeon is an expert in treating hip osteoarthritis. He or she will be able to diagnose and treat your hip, whether it is with an operation or not.
Prevention
There is no definitive method to prevent hip osteoarthritis.
There is current research being conducted between the relationship of different hip shapes and abnormalities that may lead to hip osteoarthritis such as femoroacetabular impingement.
Femoroacetabular impingement has been proposed in recent years to be a major cause of hip osteoarthritis. In fact, it seems that 1 in 4 people are predisposed to osteoarthritis due to the shape of their hip bones.
In the future, we may have ways to prevent hip osteoarthritis by dealing with the shape of your hip.
There is currently no medical evidence to show that any vitamins or minerals help in preventing osteoarthritis, such as fish oil or glucosamine.
F.A.Q. | Frequently Asked Questions
I’ve heard glucosamine and fish oils might help. Is this true?
Compared with placebo (which means a pill that does not contain any active ingredients), glucosamine, chondroitin, and their combination do not reduce joint pain or have an impact on the narrowing of joint space. This statement is based on a number of trials that have sought to answer this question.
When is the right time to have a hip replacement if I have advanced OA?
Unfortunately, there is no clear cut rule for deciding when to have a hip replacement. Some people with very severe osteoarthritis on X-rays have very limited pain and disability. Other people with only mild X-ray changes can be greatly affected by their osteoarthritis. When your hip is becoming painful, limiting your movement and stopping you from doing some of the things you’d like to be doing, such as walking, then it’s time to ask your GP if you can have a referral to an Orthopaedic surgeon. During your consult, your surgeon will discuss the pros and cons of hip replacement surgery and together you can decide if the procedure is for you.
How long does a hip replacement last?
90% last 20-30 years
What references have been used?
- Primary Osteoarthritis of the Hip: Etiology and Epidemiology. Franklin T. Hoaglund, MD, and Lynne S. Steinbach, MD. J Am Acad Orthop Surg 2001;9:320-327
- Effects of glucosamine, chondroitin, or placebo in patients with osteoarthritis of hip or knee: network meta-analysis. Wandel, Simon; Juni, Peter; Tendal, Britta; Nuesch, Eveline; Villiger, Peter M; Welton, Nicky J; Reichenbach, Stephan; Trelle, Sven. BMJ (Clinical research ed.) 2010 Sep 16. 341;c4675
- Osteoarthritis of the Hip. Nancy E. Lane, M.D. N Engl J Med 2007; 357:1413-1421October 4, 2007
- Medical management of osteoarthritis of the knee and hip joints. Rebecca Grainger and Flavia M Cicuttini. Med J Aust 2004; 180 (9): 464.
- Epidemiology of hip and knee osteoarthritis. Felson DT. Epidemiol Rev. 1988;10:1-28.
- Reichenbach S, Sterchi R, Scherer M, et al. (2007). “Meta-analysis: chondroitin for osteoarthritis of the knee or hip”. Ann. Intern. Med. 146 (8): 580–90. PMID 17438317.
